Acute Oesophageal Necrosis: A Case Report and Review Of The Literature
Sabina Beg and David Rowlands
Cite this article as: BJMP 2015;8(3):a829
|
|
Abstract Here we present a case of Acute Oesophageal Necrosis, a rare but increasingly recognised endoscopic finding. At gastroscopy distal necrosis of the oesophagus is observed. This condition is associated with a poor prognosis and therefore diagnosis should prompt aggressive correction of abnormal physiology. Abbreviations: AON - Acute Oesophageal Necrosis |
CASE
A 79 year old lady presented to the accident and emergency department with severe abdominal pain. On admission she was hypotensive and hypothermic. Blood tests demonstrated raised inflammatory markers and white count, but were otherwise unremarkable. A CT scan revealed no abnormalities. She was treated with intravenous fluids and empirical antibiotics.
She had multiple co-morbidities, including ischaemic heart disease, hypertension and chronic kidney disease.
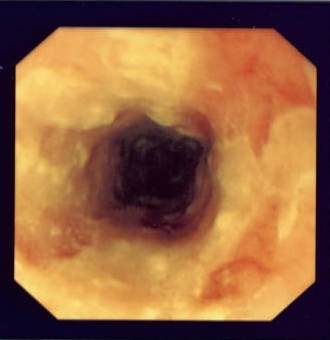
Figure 1 – Upper Oesophagus
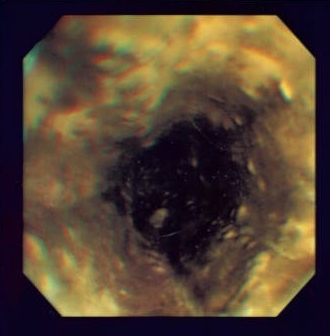
Figure 2 – Distal Oesophagus

Figure 3 - Gastro-eosophageal Junction
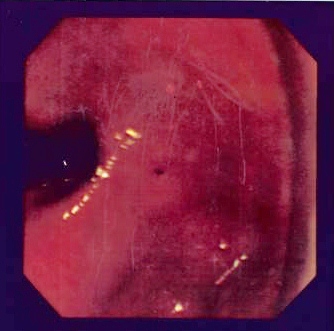
Figure 4 – Stomach (in retroflexion)
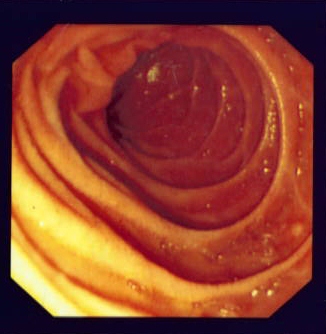
Figure 5 - Duodenum
Three days into her admission she had a single episode of hematemesis and a gastroscopy was arranged. Endoscopic features were as per figures 1- 5. Histology taken at the time showed necrotic tissue with evidence of candidiasis. Her treatment was optimised with a two-week course of fluconazole with the dose adjusted for her renal function and parenteral nutrition, with good clinical response. She was discharged after a two week hospital admission. A repeat gastroscopy 10 weeks later showed complete resolution of endoscopic features with no evidence of perforation or stricture formation.
DISCUSSION
The images seen at endoscopy demonstrate a region of oesophageal ulceration progressing to a diffuse, circumferential, black discoloration of the distal esophageal mucosa, with an abrupt transition to normal mucosa at the gastro-esophageal junction (Figs. 1-3). These endoscopic features, in the absence of a history of ingestion of caustic substances, are diagnostic of Acute Oesophageal Necrosis (AON), also known as ‘Black Oesophagus’. Whilst histology confirming necrosis is not necessary to make the diagnosis, it is confirmatory.
AON was first described in 1990 by Goldberg et al, since which over one hundred cases have been reported in the literature1. Population studies have suggested the incidence of this condition to be between 0.08% and 0.2%, although interestingly one post-mortem series of 1000 patients failed to reveal any cases2-4. There is a male preponderance, with an incidence four times greater than that for women and a peak incidence during the sixth decade of life5, 6.
The aetiology of this condition is not entirely clear; however case reports to date suggest that this is almost exclusively observed in those who are systemically unwell, usually in the context of multi-organ dysfunction5-7. It has been postulated that necrosis most commonly occurs as a consequence of hypo-perfusion caused by a low flow state in those with underlying vascular disease. This is likely to account for the predilection for the distal third of the esophagus, which is relatively less vascular5. Individual cases have occurred in association with bacterial, viral and fungal infections, whilst malnutrition, malignancy and immune-compromise appear to be important factors3, 5, 6.
The most common indication for the gastroscopy that makes the diagnosis of AON is hematemesis and melena, accounting for over 75% of cases6. It is therefore likely that AON is significantly under reported as endoscopy is often precluded in those who are clinically unstable. Further it is not clear whether hematemesis is a universal symptom of this condition; it is conceivable that AON may go undiagnosed in those in whom this is not a feature.
Whilst AON has no specific treatment, its presence is indicative of significant systemic compromise and predicts a poor prognosis. This diagnosis should alert physicians that close monitoring and aggressive treatment is required to optimise patient outcomes. There is no clear role for the use of anti-acid therapy, however this is commonly used in management due to patient symptoms, which usually includes hematemesis. Similarly, candidiasis may occur in conjunction with AON, whilst it is not thought to be causative, treatment is considered prudent given the poor prognosis associated with this condition.
For those that recover from their acute systemic insult the prognosis appears to be good. The long-term sequale of this condition includes oesophageal stenosis due to structuring. Evaluation with a repeat gastroscopy if therefore indicated if dysphagia develops.
CONCLUSION
The clinical course of AEN is variable, with an associated mortality of 32%5. The severity of the underlying clinical condition appears to be the most important factor in determining prognosis. There is no specific treatment for AON. The current body of experience suggests aggressive management of abnormal physiology optimises outcomes5, 6. Antibiotics, antifungals and nutritional support should be considered on an individual basis.
|
Competing Interests None declared Author Details SABINA BEG, BSC MBBS MRCP, North East Hertfordshire Trust, UK. DAVID ROWLANDS MBBS FRCP, North East Hertfordshire Trust, UK. CORRESPONDENCE: SABINA BEG, Lister Hospital, North East Hertfordshire NHS trust, Correy Mill lane, Hertfordshire, SG1. Email: sabina.beg@nhs.net |
References
- Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990; 98: 493 – 6.
- Ben Soussan E, Savoye G, Hochain P, e t al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002; 56: 213 – 17.
- Augusto F, Fernandes V, Cremers MI, e t al. A cute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004; 36: 411 – 15.
- Postlethwait RW, Musser AW. Changes in the esophagus in 1,000 autopsy specimens. J Thorac Cardiovasc Surg. 1974; 68:953–956.
- Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol 2010; 16: 3219 – 25.
- Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Dis Esophagus. 2006;19(2):105-10
- Gurvits GE, S hapsis A, Lau N, e t al. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007; 42: 29 – 38.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




