Acute reversible cardiomyopathy due to methamphetamine overdose
Ashok Raj Devkota, Alix Dufrense and Premraj Parajuli
Cite this article as: BJMP 2015;8(4):a830
|
|
Abstract Methamphetamine abuse is associated with various cardiac complications like acute coronary syndrome, cardiomyopathy and sudden cardiac death. We report a case of patient who presented with cardiomyopathy and acute heart failure due to intravenous methamphetamine abuse. His cardiac function recovered fully after medical management. Keywords: Methamphetamine, cardiomyopathy, heart failureAbbreviations: EKG: Electrocardiogram, ECHO: Echocardiogram, CT: Computed tomography, LVEDP: Left ventricular end diastolic pressure |
Introduction
Methamphetamine and related compounds are the most widely abused drugs in the world after cannabis 1. Methamphetamine is a synthetic stimulant which acts both on central and peripheral nervous system. It causes the release and blocks the reuptake of dopamine, norepinephrine, epinephrine and serotonin in neuronal synapse. Methamphetamine can be smoked, snorted, injected or ingested orally. Methamphetamine is more potent, and its effects last longer than cocaine 2, 3.
Methamphetamine intoxication causes various systemic complications like sympathetic over activity, agitation, seizure, stroke, rhabdomyolysis and cardiovascular collapse. Acute cardiac complications of methamphetamine like chest pain, hypertension, arrhythmias, aortic dissection, acute coronary syndrome, cardiomyopathy, and sudden cardiac death have been reported 4, 5. Chronic methamphetamine use is associated with coronary artery disease, chronic hypertension and cardiomyopathy 6.
Here we present a case of methamphetamine overdose, which presented with cardiomyopathy and severe systolic heart failure whose cardiac function was normalized after treatment.
Case presentation
A 38-year-old male presented with shortness of breath, chest tightness and sweating which started after he used intravenous crystal meth the day before presentation. He was an active poly substance abuser and used different drugs like marijuana, alprazolam, amphetamine, cocaine, percocet (oxycodone and acetaminophen) and clonazepam regularly. He was on methadone maintenance program as well. The patient did not have any cardiac problem in the past. He had a seizure disorder but he was not on medication. He had an episode of a seizure after methamphetamine use. His review of system was otherwise unremarkable.
On presentation he was tachycardic, his pulse was 128/min and his temperature was 98 degree Fahrenheit. He had bilateral diffuse crackles on lung bases. Troponin I was high 4.23 ng/ml (reference 0.01-0.05 ng/ml) and BNP was high 657 pg/ml (reference 0-100pg/ml). His electrolytes, renal function, liver function and creatinine kinase were normal. Urine toxicology was positive for opiate, methadone, amphetamine, benzodiazepine, cocaine and cannabinoid. Electrocardiogram showed sinus tachycardia at rate 130/min and QTc was prolonged at 488ms (Figure 1).
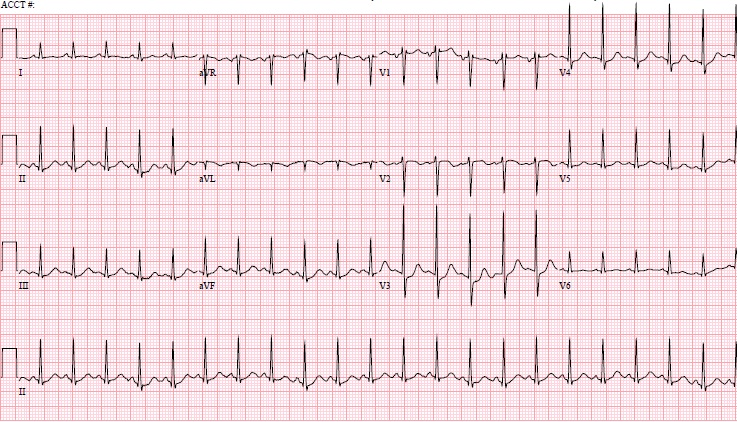
Figure 1 - Electrocardiogram: Sinus tachycardia at 130/min with prolonged QTc
Subsequently the patient became tachypnoeic and hypoxic, was intubated, put on a mechanical ventilator, and sedated with versed, fentanyl and propofol. Arterial blood showed respiratory acidosis and hypoxia. The patient was in cardiogenic shock and dopamine drip was started and intravenous Lasix was given. A subsequent chest X-ray showed newly developed pulmonary congestion. Echocardiogram showed left ventricular dilatation with diffuse hypokinesis and depressed systolic function. The left atrium was dilated. He had moderate diastolic dysfunction, mild mitral regurgitation and tricuspid regurgitation with a pulmonary artery pressure of 38mmHg. There was global left ventricular function was reduced and ejection fraction was 25-30%. His CT head was negative for an infarct or hemorrhage. He was managed in the cardiac care unit and responded very well to treatment. He became haemodynamically stable and dopamine was discontinued; aspirin, clopidogrel and carvedilol were started. The patient gradually improved and was extubated. Cardiac catheterization showed normal coronaries and normal left ventricular function. LVEDP was 18mmHg. His repeat echocardiogram one week later showed normal left ventricular systolic and diastolic function with an ejection fraction of 70%. The patient was discharged to drug rehab after eight days of treatment.
Discussion
This patient used intravenous crystal meth after which his problem started, so the most likely culprit was methamphetamine. Although he used multiple drugs including cocaine and amphetamine, which have acute and chronic effects on the heart, his cardiac function was normal before. Different mechanisms for cardiac injury due to methamphetamine have been proposed which include catecholamine excess, coronary vasospasm and ischaemia, increase in reactive oxygen species, mitochondrial injury, changes in myocardial metabolism, and direct toxic effects 3.Methamphetamine use is known to cause acute and chronic cardiomyopathy and the reversal of cardiac failure has been documented after discontinuing the drug. In one case report, a patient with chronic methamphetamine-associated cardiomyopathy did not demonstrate late gadolinium enhancement, consistent with an absence of significant fibrosis, and had left ventricular function recovered with 6 months of medical therapy and decreased drug abuse 7. Another case of a female 42 year old methamphetamine user who had transient left ventricular dysfunction and wall motion abnormalities and an index ventriculogram showed apical ballooning consistent with Takotsubo cardiomyopathy; her left ventricular function significantly improved after 3 days of medical treatment 8. In our patient, acute cardiomyopathy resolved quickly with intensive medical management. It is not clear how long it takes for cardiomyopathy to revert to normal after discontinuing the drug, or at what stage cardiac damage is irreversible. Many patients who use methamphetamine also ingest other drugs as well. It is unclear to what extent the use of multiple drugs play synergistic role in the cardiac complications that occur. Among patients who present with cardiomyopathy and cardiogenic shock, the usage of drugs like methamphetamine and co-ingestion of other drugs should be considered. Further study is needed to recommend treatment for methamphetamine and related drugs induced cardiomyopathy.
|
Acknowledgements None Competing Interests None declared Author Details ASHOK RAJ DEVKOTA, MD, Resident, Department of Internal medicine, Interfaith medical Center, Brooklyn, NY. ALIX DUFRENSE, MD, Chair, Department of Cardiology, Interfaith Medical Center, Brooklyn, NY. PREMRAJ PARAJULI, MD, Resident, Department of Medicine, Interfaith Medical Center, Brooklyn, NY. CORRESPONDENCE: ASHOK RAJ DEVKOTA, MD, Resident, Department of Internal medicine, Interfaith medical Center, 1545 Atlantic Ave, Brooklyn, NY 11213. Email: ashokdevkota@hotmail.com |
References
- World Drug Report 2012 8/21/2014; Available from: http://www.unodc.org/documents/data-and-analysis/WDR2012/WDR_2012_web_small.pdf.
- Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. 2011; Available from: http://samhsa.gov/data/2k13/DAWN2k11ED/DAWN2k11ED.htm#3.2.
- Won, S., et al., Methamphetamine-associated cardiomyopathy. Clin Cardiol, 2013. 36: p. 737-42.
- Hawley, L.A., et al., Cardiac complications of adult methamphetamine exposures. J Emerg Med, 2013. 45: p. 821-7.
- Yeo, K.K., et al., The association of methamphetamine use and cardiomyopathy in young patients. Am J Med, 2007. 120: p. 165-71.
- Kaye, S., et al., Methamphetamine and cardiovascular pathology: a review of the evidence. Addiction, 2007. 102: p. 1204-11.
- Lopez, J.E., et al., Recovery of methamphetamine associated cardiomyopathy predicted by late gadolinium enhanced cardiovascular magnetic resonance. J Cardiovasc Magn Reson, 2009. 11: p. 46.
- Srikanth, S., R. Barua, and J. Ambrose, Methamphetamine-associated acute left ventricular dysfunction: a variant of stress-induced cardiomyopathy. Cardiology, 2008. 109: p. 188-92.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




