Availability of computerised reminders in primary care doesn’t reduce heart-failure repeated hospitalisations
Luca Degli Esposti, Alessandro Filippi, Chiara Verones, Stefano Buda, Gaetano D'Ambrosio, Cinzia Germinario, Italo Paolini and PierClaudio Brasesco
Cite this article as: BJMP 2012;5(2):a518
|
|
Abstract Computerised reminders can be a support for clinical improvement. We verified their effect on heart-failure (HF) re-hospitalisation rate. |
INTRODUCTION
The widespread use of office-software in general practice makes the idea of simple, automatic computerised support an attractive one. Different tools for different diseases have been tested with mixed results, and in 2009 a Cochrane review1 concluded that “Point of care computer reminders generally achieve small to modest improvements in provider behavior. A minority of interventions showed larger effects, but no specific reminder or contextual features were significantly associated with effect magnitude”. One year later another review2 reached similar conclusion: “Computer reminders produced much smaller improvements than those generally expected from the implementation of computerised order entry and electronic medical record systems”. Despite this, simple, non-expensive, automatic reminders are frequently part of GPs’ software, even if their real usefulness is seldom tested in real life.
Repeated hospitalisation for heart failure is an important problem for every National Health System; it is estimated that about half of all re-hospitalisation could be avoided3. Adherence to guidelines can reduce re-hospitalisation rate4, and pharmacotherapy according to treatment guidelines is associated with lower mortality in the community5. In 2004 a software commonly used in Italian primary care implemented a simple reminders’ system to help GPs to improve prescription of drugs recommended for heart failure. We evaluated if this could lead to a decrease in re-hospitalisation rate.
METHODS
In 2003, using Millewin ®, a software commonly used by Italian GPs, we showed that appropriate prescription could increase using a simple pop-up reminders6; a year later, using the Italian General Practitioners database ‘Health Search – CSD Patient database (HSD) (www.healthsearch.it), we observed a lower than expected prevalence of codified diagnosis of heart failure and of prescription of both beta-blockers and ACE-Inhibitors/ARBs (data on file). Therefore in 2004 Millewin® embedded a simple reminder system to help heart failure (HF) management. The first reminder aimed to identify patients with HF, but without codified diagnosis: in case of loop diuretic and/or digoxin prescription without codified HF diagnosis a pop-up told the GP that the patients could be affected by HF and invited the physician to verify this hypothesis and eventually to record the diagnosis. The second reminder appeared when a patient with codified HF diagnosis had no beta-blocker and/or ACE-inhibitor/ARB prescription: a pop-up invited the GP to prescribe the missing drug. This reminder system was already activated in the 2004 release of the software, but required voluntary activation in the successive releases. This is a common choice in real life, where positive choices in clinical practice by software-house neither are welcomed nor accepted by GPs. We had no possibility to know who decided to keep using the reminders.
We examined the 2004-2009 HF hospitalisations in Puglia, a Southern Italian Region with a population of over 4000000, and with high HF hospitalisation rate compared with the Italian mean7. We compared the hospitalisations for patients cared for by GPs who used Millewin® in 2004 to those of the patients cared for by GPs who never used Millewin®. Data were provided by the local Health Authority, and were extracted from the administrative database.
RESULTS
We identified 64591 patients (mean age 76 y, sd 12; 49.9% men) with one or more HF hospitalisation; 17810 had > 2 hospitalisations, and were analysed for the current study.
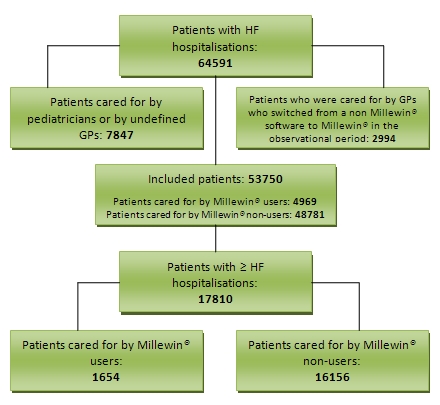
Figure 1 - Selection process leading to the identification of the patients with > 2 HF hospitalisations
The selection that led to this group is summarised in figure 1. There was no statistically significant difference between patients cared for GPs using or non using Millewin® software as far as age and gender are concerned. The re –hospitalisation rate according to the use or non-use of Millewin® of patients’ GPs is summarised in table 1.
Table 1: Re-hospitalisation rate of patients cared by Millewin® users and non-users
| Patients with ≥ 2 hospitalisation (N, %) | ||||
| Time | No MW users | MW users | Total | P |
| Within 1 year | 11260 (23.1%) | 1136 (22.9%) | 12396 (23.1%) | =N.S. |
| Within 2 years | 13851 (28.4%) | 1410 (28.4%) | 15261 (28.4%) | =N.S. |
| Within 3 years | 15144 (31.0%) | 1543 (31.1%) | 16687 (31.0%) | =N.S. |
| Within 4 years | 15803 (32.4%) | 1612 (32.4%) | 17415 (32.4%) | =N.S. |
| Within 5 years | 16083 (33.0%) | 1643 (33.1%) | 17726 (33.0%) | =N.S. |
| Within 6 years | 16156 (33.1%) | 1654 (33.3%) | 17810 (33.1%) | =N.S. |
MW = Millewin®, N.S = Not significant
The mean time before the first re-hospitalisation was 108.5 day +/- 103.3 for Millewin® non-users and 116.4 +/- 107.5 for users (p < 0.05).
DISCUSSION
Even if reasonable and clinically sound, the availability of computerised reminders aimed to help GPs to identify HF patients and to prescribe them with recommended drugs didn’t reduce re-hospitalisation rate. The first possibility to explain this result is that, after the first year, GPs didn’t re-activate the reminders’ system. Unfortunately we couldn’t verify this hypothesis, but it is known that the level of use of such a system may be low in usual care8; furthermore providers may agree with less than half of computer generated care suggestions from evidence-based CHF guidelines, most often because the suggestions are felt to be inapplicable to their patients or unlikely to be tolerated9. Epidemiological studies have shown that heart failure with a normal ejection fraction is now a more common cause of hospital admission than systolic heart failure in many parts of the world10-11. Despite being common, this type of heart failure is often not recognised, and evidence based treatment—apart from diuretics for symptoms—islacking12. It is therefore possible that increasing ACE-I/ARBs and beta-blockers use in these patients doesn’t influence the prognosis and hospitalisation rate. Unfortunately administrative databases do not permit to distinguish the characteristic of HF. We must also consider that the use of appropriate drugs after HF hospitalisation could spontaneously increase in the last years; a survey in Italian primary care showed that 87% of HF patients used inhibitors of the renin-angiotensin system, and 33% beta-blockers13. A further relevant increase in ACE-I/ARBS is therefore unlikely, while a improvement is clearly needed for beta-blockers. Could more complex and information-providing reminders be more useful? This is unlikely since adding symptom information to computer-generated care suggestions for patients with heart failure did not affect physician treatment decisions or improve patient outcomes14. Furthermore, consultation with a cardiologist for starting beta-blocker treatment is judged mandatory by 57% of Italian GPs13, thus reducing the potential direct effect of reminders on prescription. Finally we must remember that part of the hospitalisation due to HF worsening can be due to non-cardiac disease, such as pneumonia, anemia, etc; all these cause cannot be affected by improved prescription of cardiovascular drugs.
Albeit simple and inexpensive, computerised reminders aren’t a neutral choice in professional software. Too many pop-ups may be disturbing and may lead to systematic skipping the reminders’ text. This can be a problem, since computerised reminders have proved to be useful for other important primary-care activity, such as preventive interventions15. In our opinion, at the moment, a computerised reminder-system should be proposed only as a part of a more complex strategy, such as long-term self or group audit and/or pay for performance initiative.
CONCLUSIONS
Availability of computerised automatic reminders aimed to improve detection of heart-failure patients and prescription of recommended drugs doesn’t decrease repeated hospitalisation; these tools should be probably tested in the context of a more complex strategy, such as a long-term audit.
|
Competing Interests None declared Author Details LUCA DEGLI ESPOSTI, EconD, CliCon S.r.l. Health, Economics and Outcomes Research. Ravenna, Italy. ALESSANDRO FILIPPI, MD, General Practitioner, Italian College of General Practitioners, Firenze, Italy. CHIARA VERONESI, StatD, CliCon S.r.l. Health, Economics and Outcomes Research. Ravenna, Italy. STEFANO BUDA, ElEng, CliCon S.r.l. Health, Economics and Outcomes Research. Ravenna, Italy. GAETANO D'AMBROSIO, MD, General Practitioner, Italian College of General Practitioners, Firenze, Italy. CINZIA GERMINARIO, PhD, Department of Biomedical Sciences, Hygiene Section, University of Bari Aldo Moro, Bari, Italy. ITALO PAOLINI, MD, General Practitioner, Italian College of General Practitioners, Firenze, Italy. PIERCLAUDIO BRASESCO, MD, General Practitioner, Italian College of General Practitioners, Firenze, Italy. CORRESPONDENCE: LUCA DEGLI ESPOSTI, CliCon S.r.l., Via Salara, 36, 48100, Ravenna, Italy. Email: luca.degliesposti@clicon.it |
References
- Shojania KG, Jennings A, Mayhew A, et al. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No.: CD001096. DOI: 10.1002/14651858.CD001096.pub2.
- Kaveh G. Shojania, Alison Jennings, Alain Mayhew RPT, et al. Effect of point-of-care computer reminders on physician behavior: a systematic review CMAJ 2010. DOI:10.1503/cmaj.090578.
- Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med. 1998 May 25;158(10):1067-72.
- Komajda M, Lapuerta P, Hermans N, et al. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. Eur Heart J. 2005 Apr 12.
- Störk S, Hense HW, Zentgraf C, et al. Pharmacotherapy according to treatment guidelines is associated with lower mortality in a community-based sample of patients with chronic heart failure: a prospective cohort study. Eur J Heart Fail.2008 Dec;10(12):1236-45.
- Filippi A, Sabatini A, Badioli L, et al. Effects of an automated electronic reminder in changing the antiplatelet drug-prescribing behavior among Italian general practitioners in diabetic patients: an intervention trial. Diabetes Care. 2003 May;26(5):1497-500.
- Ministero della Salute. Rapporto Nazionale di Monitoraggio dei Livelli Essenziali di Assistenza. Anno 2007-2009. Novembre 2011. (http://www.salute.gov.it/imgs/C_17_pubblicazioni_1674_allegato.pdf).
- Nikki Rousseau, Elaine McColl, John Newton, et al. Practice based, longitudinal, qualitative interview study of computerised evidence based guidelines in primary care bmj.com 2003;326:314.
- Brian Keeffe, Usha Subramanian, William M. et al. Provider Response to Computer-Based Care Suggestions for Chronic Heart Failure Med Care 2005;43: 461–465.
- Sanderson JE. Heart failure with a normal ejection fraction. Heart 2007;93:155-8.
- Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006;355:251-9.
- John E Sanderson, Gabriel W K Yip.Heart failure with normal ejection fraction BMJ 2009;338:b52.
- Tarantini L, Cioffi G, Pulignano G, et al. Heart failure in primary care in Italy: analysis of management and needs by general practitioners. G Ital Cardiol (Rome). 2010 Sep;11(9):680-7.
- Subramanian U, Fihn SD, Weinberger M, et al. A controlled trial of including symptom data in computer-based care suggestions for managing patients with chronic heart failure. Am J Med. 2004 Mar 15;116(6):375-84.
- Timothy S. Loo, Roger B. Davis, Lewis A. et al. Electronic Medical Record Reminders and Panel Management to Improve Primary Care of Elderly Patients Arch Intern Med. 2011;171(17):1552-1558.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




