Can telephone triage in primary care help in earlier diagnosis of cancer?
Ejaz Mahmood, Jonathan Griffiths & Yuhua Su.
Cite this article as: BJMP 2017;10(1):a1005
|
|
Abstract Aims: One of the main focus points in General Practice is to identify symptoms and signs of cancers for early diagnosis to improve outcomes. Our study aims to assess if telephone triage helped in prioritising early assessment and referral of patients who were diagnosed with a cancer. Abbreviations: GP- General Practitioner. |
Introduction
Telephone triage has been used by many practices in primary care to manage workload and prioritise patients for same day appointments.1,2 Telephone triage may have benefits in terms of managing work load,3 but is also associated with certain risks,4 which has worried both clinicians and patients.5 The analysis of the use of telephone triage has so far focused on the ease of access, demand management, cost effectiveness, quality of consultations, safety and patient satisfaction. However, other effects in terms of patient outcome may exist. One of the main focuses in General Practice is to identify symptoms and signs of cancer for early diagnosis to improve outcome. Our study aims to assess whether telephone triage helps in prioritising early assessment and referral of patients who are subsequently diagnosed with cancer.
Methods
A retrospective analysis of all the patients at our practice who had a diagnosis of cancer made between April 2013 and December 2014 was carried out.
Patients have a choice of 2 different ways to book an appointment in our practice.
- Telephone triage for same day appointment requests, where a triaging doctor decides about the urgency of a problem and books the appointment, arranges tests or gives advice after speaking to patients over the phone. This group is referred as “Group 1” in this study.
- Patients book the next available appointment to see a GP through reception without any triage. This group is referred to as “Group 2” in this study.
The date of first contact with the GP practice for the symptoms which later lead to a diagnosis of cancer was noted for both groups. This was the telephone triage date for the first group and the date the appointment was booked by the patients for the second group. The date the patient was first seen in secondary care for further assessment and investigations was also noted. The duration between first contact with GP practice and GP appointment, and the duration between the first contact with practice and first hospital appointment were calculated. This information was gathered from practice computer records.
Patients who were diagnosed with cancer through screening were excluded. Slow growing tumours which do not merit a 2-week rule referral, such as basal cell cancer of skin were excluded. Patients whose appointments were initiated by the GP on reviewing the results of routine tests were not included. Patients diagnosed with cancer in hospital without going through primary care referral were also excluded from this study.
There are two research questions:
- Is there a significant difference in the time required from the first contact with primary care to the GP Clinic appointment between Group 1 and Group 2 patients?
- Is there a significant difference in the time required from the first contact with primary care to the date the patient was seen in the secondary care between Group 1 and Group 2 patients?
Descriptive statistics (such as the mean, standard deviation, median, minimum, and maximum) were used to present the time required from the first contact with primary care to the GP Clinic appointment; and the time required from the first contact with primary care to the date patient seen in the hospital, for Group 1 and Group 2 patients. Wilcoxon rank-sum test was used to answer each research question. A p-value less than 0.05 indicated significance at the 0.05 level.
All data analyses were conducted using SAS.
Results
A total number of 39 patients were included in the study. Among them, 13 (33%) used telephone triage to make their appointments and 26 (67%) booked their appointment by themselves.
Figure 1 shows the bar charts of the time required from the first contact to GP practice, to the GP clinic appointment for Group 1 and Group 2 patients. It took 0-3 days for 12 Group 1 patients and 8-11 days for 1 Group 1 patient. The time required from the first contact to GP practice to the GP Clinic appointment for Group 2 patients can be illustrated by the same manner.
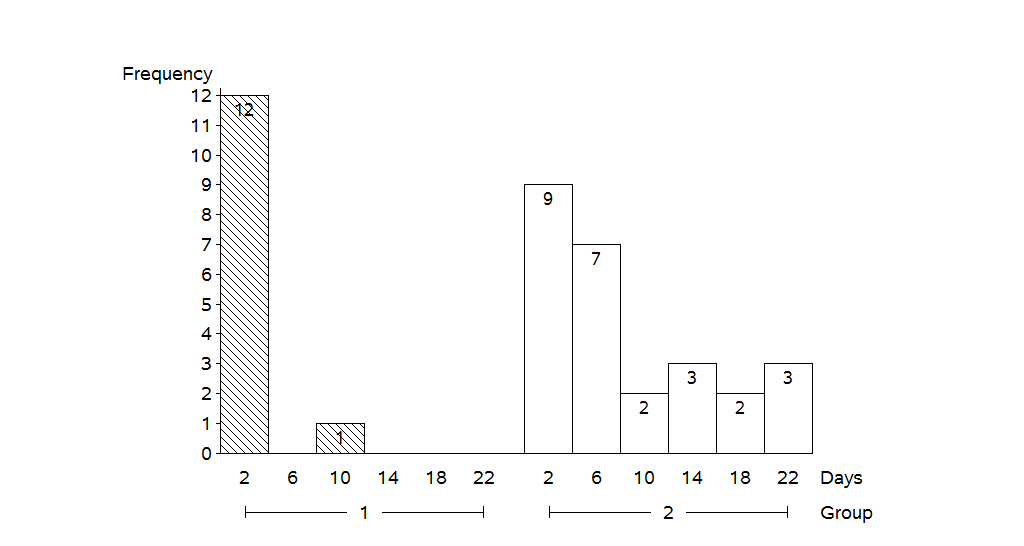
Figure 1: Bar charts of the time (days) required from the first contact for surgery to the GP Clinic appointment for Group 1 and Group 2 patients. (Note that the midpoints 2, 6, 10, 14, 18, and 22 represented days within the range of 0-3, 4-7, 8-11, 12-15, 16-19, and 20-23, respectively.)
Table 1 shows the summary statistics for the time (days) required from the first contact with the practice, to the GP Clinic appointment for Group 1 and Group 2 patients. The average time required was 0.77 days for Group 1 patients and the average time required for Group 2 patients was 7.88 days. The results of Wilcoxon rank-sum test indicated that this was a statistically significant difference in time required from the first contact for surgery to the GP Clinic appointment between Group 1 patients (patients using Telephone triage to make their appointments) and Group 2 patients (patients booking their appointment by themselves) (p = 0.0020).
| Number | Mean | SD | Median | Min | Max | |
| Group 1 | 13 | 0.77 | 2.24 | 0 | 0 | 8 |
| Group 2 | 26 | 7.88 | 7.53 | 6 | 0 | 23 |
Table 1:Summary statistics for the time (days) required from the first contact for surgery to the GP Clinic appointment for Group 1 and Group 2 patients. SD = standard deviation.
Figure 2 shows the bar charts of the time required from the first contact with the GP practice, to the date patients were seen in the secondary care for Group 1 and Group 2 patients. It took 0-5 days for 4 Group 1 patients, 10-19 days for 5 Group 1 patients, 20-29 days for 1 Group 1 patient, 30-39 days for 2 Group 1 patients, and 90-99 days for 1 Group 1 patient. The time required from the first primary care contact to the date patient seen in the secondary care for Group 2 patients can be illustrated by the same manner.
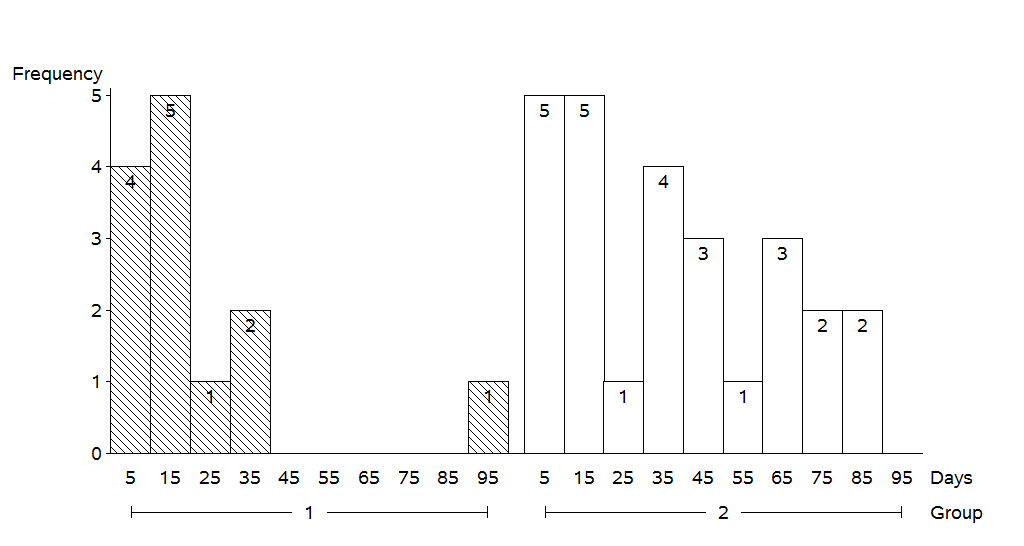
Figure 2: the bar charts of the time required from the first contact for surgery to the date patient seen in the hospital for Group 1 and Group 2 patients. (Note that the midpoints 5, 15, 25, 35, 45, 55, 65, 75, 85 and 95 represented days within the range of 0-9, 10-19, 20-29, 30-39, 40-49, 50-59, 60-69, 70-79, 80-89 and 90-99, respectively).
Table 2 shows the summary statistics for the time (days) required from first contact with GP practice to the date patients were seen in the hospital for Group 1 and Group 2 patients. The average time required for Group 1 patients was 19.54 days and the average time required for Group 2 patients was 35.69 days. The results of Wilcoxon rank-sum test indicated that this was a statistically significant difference in time required from the first contact to the primary care to the date patient seen in the hospital between Group 1 patients (patients using Telephone triage to make their appointments) and Group 2 patients (patients booking their appointment by themselves) (p = 0.0474).
| Number | Mean | SD | Median | Min | Max | |
| Group 1 | 13 | 19.54 | 23.41 | 10.00 | 3 | 90 |
| Group 2 | 26 | 35.69 | 26.28 | 32.50 | 1 | 88 |
Table 2: Summary statistics for the time (days) required from the first contact for surgery to the date patient seen in the hospital for Group 1 and Group 2 patients. SD = standard deviation.
| Type of Cancer | Number of Patients |
| Lung | 5 |
| Breast | 5 |
| Colorectal | 4 |
| Malignant melanoma of Skin | 3 |
| Squamous Cell carcinoma of Skin | 3 |
| Oesophagous | 2 |
| Stomach | 2 |
| Urinary Bladder | 2 |
| Larynx | 2 |
| Pancreas | 1 |
| Endomtrium | 1 |
| Cervix | 1 |
| Kidney | 1 |
| Prostate | 1 |
| Testis | 1 |
| Tonsil | 1 |
| Lymphoma | 1 |
| Appendix | 1 |
| Myelodysplastic | 1 |
| Olfactory Neuroblastoma | 1 |
Table 3: Number of patients with types of cancer.
Discussion
More than 90% of contacts with healthcare in the UK occur in primary care.6 The estimated numbers of consultation for a typical practice in England rose from 21,100 in 1995 to 34,200 in 2008 as per analysis conducted by Hippisley-Cox J et al.7 With increasing demands being placed upon General Practice, there is a need to explore innovative ways of working which enable the prioritisation of patients with concerning symptoms. Telephone triage has been considered to reduce the demand for face-to-face consultation with GPs,3 which can potentially free up time for effective use. NHS England report ‘Transforming Urgent and Emergency Care Service in England’ suggests GPs should offer more telephone consultations to reduce pressure on accident and emergency.8 However, a cluster-randomised controlled trial (The Esteem Trial) across 42 practices showed that telephone triage increased the number of primary care contacts in the following 28 days, after patients’ request for same day GP consultation.1
With increasing demands for consultations, it is important to have a system to identify and prioritise patients for early assessment; who may have a suspected cancer diagnosis. Our study demonstrates that telephone triage reduces the time from first primary care contact to face to face assessment in primary and secondary care for patients with suspected cancer. Patient numbers are small and the sample is from one practice, yet the difference seen is statistically significant.
Cancer stage at diagnosis is one of the major reasons for difference in cancer survival in different countries.9,10 The delay in cancer diagnosis can be due to multiple factors. Telephone triage can provide an opportunity to patients to discuss symptoms early with a GP, and this can reduce delays in the cancer diagnosis pathway. It has been shown that certain alarm symptoms are associated with the likelihood of cancer diagnosis 11 and these can be used to prioritise the patients in triage process. It may also reduce anxiety amongst patients waiting for an appointment, who are concerned about their symptoms.
Telephone triage should not only be seen as a way of managing demands and appointments but also as a system to improve patient outcome. Further research is clearly needed on a larger scale to determine if the results are reproducible in other settings as patients’ knowledge and understanding about cancer warning symptoms and healthcare seeking behaviour may vary among different population sets.
|
Acknowledgements ANGELA ROBERTS, Practice Development Manager, Swallow Medical Centre. Competing Interests None declared Author Details EJAZ MAHMOOD, MBBS, MRCGP, Swanlow Medical Centre, Dene Drive, Winsford, CW71AT, UK. JONATHAN GRIFFITHS, MBChB, MRCGP, Swallow Medical Centre, Dene Drive, Winford, CW71AT, UK. YUHUA SU, PhD IN STATISTICS, Dr. Su Statistics, Kaunakakai, Hawaii, USA. CORRESPONDENCE: EJAZ MAHMOOD, 1325, Osbourne Avenue, Roslyn, PA 19001. USA Email: ejazmahmood78@gmail.com |
References
- Campbell JL, Fletcher E, Britten N, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. The Lancet. 2014;384(9957):1859-68.
- McKinstry B, Walker J, Campbell C, et al. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. British Journal of General Practice. 2002;52(477):306-10.
- Jiwa M, Mathers N, Campbell M. The effect of GP telephone triage on numbers seeking same-day appointments. The British Journal of General Practice. 2002;52(478):390-391.
- Katz HP, Kaltsounis D, Halloran L, et al.Patient safety and telephone medicine. Journal of general internal medicine. 2008;23(5):517-22.
- McKinstry B, Watson P, Pinnock H, et al. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. The British Journal of General Practice. 2009;59(563):e209-e218.
- Rubin G, McPhail S, Elliott K. National audit of cancer diagnosis in primary care. Royal College of General Practitioners. 2011.
- Hippisley-Cox J, Fenty J, Heaps M. Trends in Consultation Rates in General Practice 1995 to 2006: Analysis of the QRESEARCH database. London: QRESEARCH and The Information Centre for health and social care. 2007.
- NHS England. Transforming urgent and emergency care services in England. Urgent and emergency care review. End of phase 1 report. 2013. http://www.nhs.uk/NHSEngland/keogh-review/Documents/UECR.Ph1Report.FV.pdf
- Coleman M, Forman D, Bryant H, et al. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. The Lancet. 2011;377(9760):127-38.
- Gatta G, Capocaccia R, Sant M, et al. Understanding variations in survival for colorectal cancer in Europe: a EUROCARE high resolution study. Gut. 2000;47(4):533-8.
- http://www.nice.org.uk/guidance/ng12/resources/suspected-cancer-recognition-and-referral-1837268071621

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




