Cervical ripening balloon as an alternative for induction of labour: a randomized controlled trial
Toh Lick Tan, Grace Yang Huang Ng, Sheri Ee-Lin Lim, Shephali Tagore, Ei Ei Phyo Kyaw and George Seow Heong Yeo
Cite this article as: BJMP 2015;8(1):a806
|
|
Abstract Objective: To evaluate the use of cervical ripening balloon (CRB) for induction of labour (IOL) in Singapore. |
Introduction
Increasing number of term deliveries undergo induction of labour (IOL). This figure is as high as 1 in 4 in developed countries, making it one of the most common procedures a woman may experience in pregnancy. 1 IOL may be achieved with pharmacological, mechanical or surgical methods. 1, 2 Mechanical methods were the first methods used to ripen the cervix and induce labour. The National Institute of Clinical Excellence (NICE) does not recommend the routine use of mechanical methods for IOL as only heterogeneous small studies were available at their time of publication more than half a decade ago. 2 However, since then there is increasing evidence of safety and efficacy of mechanical IOL. Subsequent publications including those from World Health Organization (WHO) and Cochrane Database of Systematic Reviews support the use of balloon catheter for IOL. 1, 3 It is therefore important to revisit the role of mechanical methods of IOL.
The Cochrane Database of Systematic Reviews concluded that mechanical methods of induction of labour have a lower risk of uterine hyperstimulation with similar caesarean section rates and delivery within 24 hours as prostaglandins. Furthermore, mechanical methods reduce the risk of caesarean section when compared with oxytocin induction of labour. 3 This review is consistent with another earlier systematic review. 4
Both Pfizer’s Prostin (PGE) and Cook Medical’s Cervical Ripening Balloon (CRB) are licensed for IOL. While the use of Prostin is a standard care in Singapore, the CRB has not been used routinely. We therefore propose a study to evaluate the use of CRB for IOL in Singapore.
Methods
A prospective cohort randomised controlled study was conducted in a tertiary referral maternity unit in Singapore. Pregnant women aged 21 – 40 years old with a singleton pregnancy with no major fetal anomaly who were suitable for vaginal delivery and scheduled for a planned IOL at 37+0 to 41+6 weeks gestation were invited for the study. Cases were excluded if at the start of the planned IOL, they were in spontaneous labour, had a cervical dilatation of ³3 cm, had confirmed rupture of membrane, had abnormal cardiotocogram (CTG), had a scarred uterus such as previous caesarean section, had malpresentation in labour, or if caesarean section delivery was indicated. Women who were unable to give or had withdrawn their consent to participate in the trial were also excluded for the study.
All suitable pregnant women receiving team care who require elective IOL were identified in antenatal clinic, antenatal or labour wards by the attending doctor or clinical research coordinator (CRC). Following routine counselling for IOL by the attending doctor, the woman will be offered participation in the study and a member of the research team will counsel and obtain informed consent from her. The woman will be made to understand that participation in the study is voluntary, does not affect her medical care and consent for participation can be withdrawn at any stage of the study. Women who were uncertain in their participation were offered the opportunity to participate during her follow-up or on the day of IOL after further consideration. Patient information leaflet on IOL as well as information of the study were made available to the participants.
On the day of the IOL, the participants were reviewed for the appropriateness of the IOL and participation in the study. A presentation scan, vaginal examination for cervical dilatation and CTG were performed. If they were suitable, they were randomly allocated PGE or CRB IOL in labour ward. Randomization was achieved with third party sealed envelope allocation. A total of 75 envelopes containing a folded paper with the words “Cervical Ripening Balloon” and another 75 identical envelopes containing a folded paper with the word “Prostin” were prepared and shuffled after sealing. These randomized envelopes were then labelled sequentially with their randomization allocation number from 1 to 150. The participants who underwent randomization were allocated to the next randomization allocation numbered envelop which contain either allocation for CRB or PGE IOL.
Participants undergoing CRB IOL will have the CRB inserted after cleaning the vulva and vagina with Cetrimide solution. The uterine and vaginal balloons of the CRB will be gradually inflated with normal saline, initially 40 ml and 20 ml respectively, and a further 20 ml each hour later until each balloon is 80 ml. CTG monitoring was undertaken before and after each inflation for at least 20 minutes. If the participant was not in labour after complete inflation of the balloons, she would be transferred to the antenatal wards for rest before removing the CRB 12 hours after insertion in labour ward when possible.
Participants undergoing PGE IOL will have 3 mg Prostin tablet inserted in the posterior fornix after cleaning the vulva with Cetrimide solution. CTG monitoring was also undertaken for at least 40 minutes after PGE insertion. If the participant was not in labour, she would be transferred to the antenatal wards. If there was no response to the first PGE, a repeat dose was given after 6 hours in labour ward when possible.
Participants will undergo artificial rupture of membrane (ARM) and/or oxytocin infusion augmentation of labour as necessary. If the participant was not in labour or ARM was not possible after removing the CRB or 2 cycles of PGE, the participant would have been considered having a failed IOL and will leave the study protocol with her subsequent management determined by the specialist attending to her. This would typically involve insertion of a third or first PGE in the PGE or CRB arm respectively.
Upon delivery of the pregnancy, a member of the research team will interview the participant and obtain demographics, labour and delivery outcomes data from the clinical notes. Pain and maternal satisfaction scores and comments were also recorded by interviewing the participants in the post-natal period; these findings will however be discussed separately.
The data was collected on a pro forma and entered into an excel spreadsheet. The data was then analysed using IBM SPSS Statistics version 19.
This study was approved by the SingHealth centralised institutional review board with the reference number of 2013/553/D.
Results
A total of 138 women were approached to join the study but 40 (29.0%) women declined. There was no significant difference in maternal age (27.8 ± 5.4 vs 28.7 ± 5.2 years; p = 0.373), ethnicity, proportion of primigravidae (62.5% vs 53.1%; p = 0.349), weight (61.2 ± 15.4 vs 64.4 ± 13.8 kg; p = 0.228), BMI (24.8 ± 5.8 vs 25.3 ± 5.0 kg/m2; p = 0.646) and primary indication for IOL between women who declined and accepted enrolment to the study respectively.
The remaining 98 women were enrolled for the study. Eight-seven women were randomized after excluding 6 women in spontaneous labour, 1 woman with non-cephalic fetal presentation, and 1 woman had confirmed ruptured of membrane on admission for their IOL, as well as 3 other cases in which the women presented for IOL without the availability of the research team (figure 1).
Figure 1. Flow diagram of recruitment, randomisation and completion status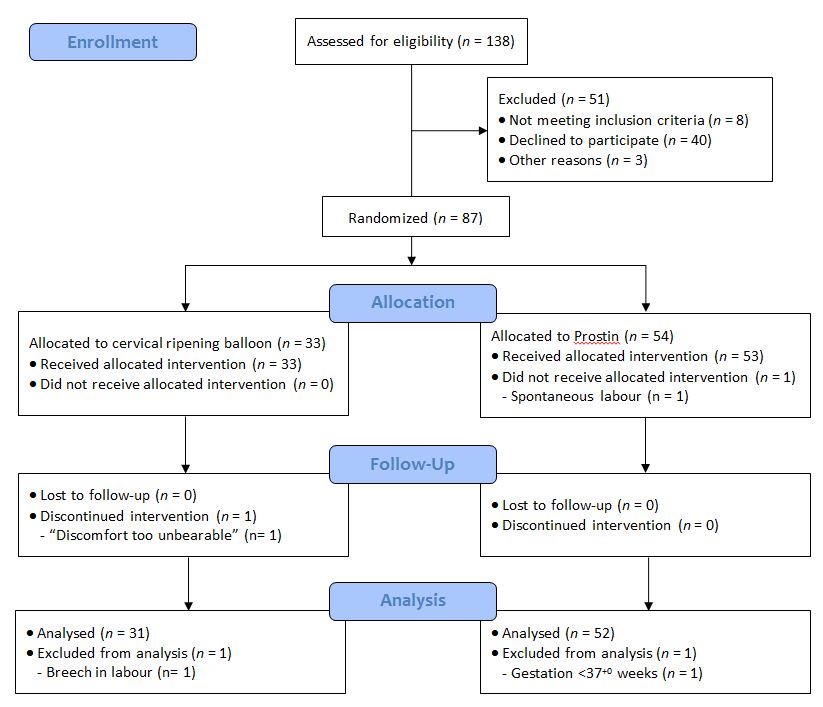
In the CRB arm, one woman withdrew from the study after 8 hours 55 minutes as she felt the discomfort was too unbearable. Another woman was excluded when she was found to have spontaneous version to breech in labour. One woman randomized to PGE did not receive it as she went into spontaneous labour prior to IOL. Another woman in the PGE arm was subsequently found to be only 36+3 weeks and was therefore excluded from analysis (figure 1). The remaining 83 cases were analysed and their characteristics are shown in table 1.
The induction to vaginal delivery time, as well as, vaginal delivery rate were similar in both arms of the study (table 2). Compared to PGE arm, participants undergoing CRB IOL were faster in achieving cervical dilatation ≥4 cm (14.4 ± 5.7 vs 23.5 ± 16.6 hr; p = 0.001) and requesting epidural (16.4 ± 5.4 vs 23.2 ± 15.8 hr; p = 0.040), as well as more likely to require oxytocin infusion for augmentation (77.4% vs 50.0%; p = 0.020). Uterine hyperstimulation defined as >5 contractions every 10 minutes was only found in PGE arm. Cervical dilatation from 0 – 2 cm to ≥4 cm was achieved without regular contractions in 2 (6.9%) cases in the CRB arm and 1 (2.4%) case in the PGE arm. The mean frequency of uterine contractions at cervical dilatation ≥4 cm was 2.5 ± 1.4 in 10 minutes for CRB arm compared to 3.8 ± 1.4 in 10 minutes for PGE arm (p <0.001). No case of uterine rupture was observed.
There was 1 (3.2%) case for failed CRB IOL where both uterine and cervical balloons were found in the vagina suggesting that either placement of the uterine balloon was not optimal or it was expelled after placement. The woman went on to have Prostin and delivered vaginally. In the 9 (17.3%) cases in the PGE group that did not respond after 2 cycles, all went on to have the third Prostin successfully except for 2 women who required Caesarean section for persistent failed IOL.
The birth outcomes of both arms of the study were also similar with no case of stillbirth (table 3). There were 2 case of neonatal intensive care unit admission in the PGE arm for continuous positive airway pressure therapy; both were discharged from NICU within 24 hours.
Table 1. Characteristics of participants undergoing cervical ripening balloon (CRB) and Prostin (PGE) induction of labour.
| CRB (n = 31) | PGE (n = 52) | p | |||
| Maternal age, years (83) 1 | 28.2 | ± 5.3 | 28.7 | ± 5.0 | 0.646 |
| Ethnicity (83) 2 | 0.222 | ||||
| · Chinese | 35.5% | (11) | 42.3% | (22) | |
| · Malay | 54.8% | (17) | 36.5% | (19) | |
| · Indian | 3.2% | (1) | 15.4% | (8) | |
| · Others | 6.5% | (2) | 5.8% | (3) | |
| Primigravidae (83) 2 | 61.3% | (19) | 44.2% | (23) | 0.174 |
| Weight, kg (83) 1 | 64.4 | ± 15.0 | 63.9.4 | ± 13.2 | 0.861 |
| BMI, kg m-2 (83) 1 | 25.5 | ± 5.0 | 25.0 | ± 5.1 | 0.706 |
| Pre delivery Hb, g dl-1 (80) 1 | 11.6 | ± 1.8 | 12.0 | ± 1.3 | 0.211 |
| GBS positive (79) 2 | 22.6% | (7) | 21.2% | (11) | 0.204 |
| Gestational age, weeks (83) 1 | 39.4 | ± 1.1 | 39.2 | ± 1.9 | 0.357 |
| Cervical dilatation, cm (83) 1 | 1.0 | ± 0.7 | 0.9 | ± 0.7 | 0.954 |
| Primary indication for IOL (83) 2 | 0.108 | ||||
| · Decreased fetal movement 3 | - | 11.5% | (6) | 0.082 | |
| · Post dates 3 | 54.8% | (17) | 32.7% | (17) | 0.065 |
| · Gestational diabetes 3 | 16.1% | (5) | 13.5% | (7) | 0.756 |
| · Impending macrosomia 3 | - | 1.9% | (1) | 0.526 | |
| · IUGR 3 | 3.2% | (1) | - | 0.137 | |
| · Low amniotic fluid index 3 | 19.4% | (6) | 34.6% | (18) | 0.089 |
| · Maternal request 3 | 3.2% | (1) | 5.8% | (3) | 0.489 |
| · Pre-eclampsia 3 | 3.2% | (1) | - | 0.373 | |
1 Values are mean ± SD, p calculated with Student t-test; 2 Values are percentage (n), p calculated with Pearson chi-square test; 3 Values are percentage (n), p calculated with Fisher’s exact test.
Table 2. Labour outcomes of participants undergoing cervical ripening balloon (CRB) and Prostin (PGE) induction of labour.
| CRB (n = 31) | PGE (n = 52) | p | |||
| IOL to ≥4 cm dilatation, hr (78) 1 | 14.4 | ± 5.7 | 23.5 | ± 16.6 | 0.001 |
| IOL to full dilatation, hr (66) 1 | 20.8 | ± 6.1 | 24.8 | ± 15.7 | 0.150 |
| IOL to vaginal delivery, hr (63) 1 | 21.2 | ± 6.8 | 25.6 | ± 16.1 | 0.136 |
| Duration of 2nd stage, hr (63) 1 | 0.9 | ± 2.9 | 0.8 | ± 0.9 | 0.741 |
| Delivery within 24 hr (83) 2 | 77.3% | (17) | 61.0% | (25) | 0.265 |
| Failed IOL (83) 3 | 3.2% | (1) | 17.3% | (9) | 0.082 |
| Number of PGE used (83) 2 | <0.001 | ||||
| · 0 | 96.8% | (30) | - | ||
| · 1 | 3.2% | (1) | 53.8% | (28) | |
| · 2 | - | 28.8% | (15) | ||
| · 3 | - | 17.3% | (9) | ||
| Augmentation use (83) 3 | 77.4% | (24) | 50.0% | (26) | 0.020 |
| Epidural use (83) 3 | 58.1% | (18) | 55.8% | (29) | 1.000 |
| · IOL to epidural use, hr (47) 1 | 16.4 | ± 5.4 | 23.2 | ± 15.8 | 0.040 |
| · Epidural use to delivery, hr (47) 1 | 9.2 | ± 4.1 | 7.0 | ± 3.8 | 0.065 |
| Contractions 1 | |||||
| · At IOL (83) | 0.2 | ± 0.6 | 0.2 | ± 0.5 | 0.579 |
| · 3 hr after IOL (81) | 2.0 | ± 1.9 | 1.6 | ± 1.9 | 0.451 |
| Contractions >5 every 10 min 3 | |||||
| · 30 min after IOL (81) | - | - | - | ||
| · 3 hr after IOL (81) | - | 2.0% | (1) | 1.000 | |
| Vaginal delivery (83) 3 | 71.0% | (22) | 78.8% | (41) | 0.438 |
| Indication for LSCS (20) 2 | 0.513 | ||||
| · Failed IOL | - | 18.2% | (2) | ||
| · FTP in 1st stage of labour | 55.6% | (5) | 36.4% | (4) | |
| · FTP in 2nd stage of labour | 22.2% | (2) | 9.1% | (1) | |
| · NRFS | 11.1% | (1) | 27.3% | (3) | |
| · FTP and NRFS | 11.1% | (1) | 9.1% | (1) | |
1 Values are mean ± SD, p calculated with Student t-test; 2 Values are percentage (n), p calculated with Pearson chi-square test; 3 Values are percentage (n), p calculated with Fisher exact test.
Table 3. Birth outcomes of participants undergoing cervical ripening balloon (CRB) and Prostin (PGE) induction of labour.
| CRB (n = 31) | PGE2 (n = 52) | p | |||
| Male fetus (83) 2 | 51.6% | (16) | 42.3% | (22) | 0.496 |
| Birth weight, g (83) 1 | 3,166 | ± 478 | 3,094 | ± 417 | 0.472 |
| Apgar at 5 min <7 (83) | - | - | - | ||
| Meconium aspiration (83) | - | - | - | ||
| Pyrexia in labour (83) 3 | 6.5% | (2) | 5.8% | (3) | 1.000 |
| NICU admission (83) 2 | - | 3.8% | (2) | 0.526 | |
| ITU admission (83) | - | - | - | ||
1 Values are mean ± SD, p calculated with Student t-test; 2 Values are percentage (n), p calculated with Pearson chi-square test; 3 Values are percentage (n), p calculated with Fisher exact test.
Discussion
To the best of our knowledge, this is the first randomized controlled study to assess the use of CRB for IOL in Singapore. Our study concur with the published literature that both CRB and PGE have similar rate of vaginal deliveries and rate of deliveries within 24 hours. Both methods are effective and safe with PGE having a higher risk of uterine hyperstimulation and need for Caesarean section for failed IOL.
Pharmacological induction of labour using PGE is the most established form of IOL. However, it is important to be able to offer alternative methods to women particularly in cases of hypersensitivity or allergy to PGE. PGE can cause bronchospasm complicating asthma, a medical condition which affects 4 – 12% of pregnant women. 5, 6 Similarly, caution should be exercised in the use of PGE in women with other common medical conditions such as hypertension and epilepsy.
In addition, women may not respond to PGE for IOL, or the PGE may only result in uterine tightenings which do not lead to cervical dilatation. In these situations the CRB may be considered as an adjunct for IOL to avoid Caesarean section of ‘failed IOL’.
The risk of uterine hyperstimulation and the need for a repeat dose in 6 to 8 hours for PGE typically require the women to be admitted for IOL. The use of CRB does not require planned intervention until 12 hours later. This potentially allows an outpatient IOL if further studies support its safety in this aspect.
The application of PGE is relatively straightforward and is already performed by both doctors and midwives. The insertion of CRB may however be considered too invasive for midwives thus limiting the type and hence availability of staff to commence IOL. We have explored the learning curve in the insertion of CRB and will discuss this separately.
Conclusion
Both CRB and PGE are effective methods for IOL at term. Each method has its own benefits and limitations. The availability of both methods in an obstetric unit will allow the clinician to choose the most appropriate form of IOL, provide a complementary method of IOL, as well as offer women choice in their IOL.
|
Acknowledgements We are grateful for the supply of cervical ripening balloons for the study provided by Cook Medical. Competing Interests None declared Author Details TOH LICK TAN , MBBS MRCOG, Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore. GRACE YANG HUANG NG, MBChB, Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore. SHERI EE-LIN LIM, MBBS PhD MRCOG, Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore. SHEPHALI TAGORE, MBBS MRCOG, Department of Maternal Fetal Medicine, KK Women’s and Children’s Hospital, Singapore. EI EI PHYO KYAW, BDS, BSc (Hons) , Department of Maternal Fetal Medicine, KK Women’s and Children’s Hospital, Singapore. GEORGE SEOW HEONG YEO, MBBS FRCOG FAMS, Department of Maternal Fetal Medicine, KK Women’s and Children’s Hospital, Singapore. CORRESPONDENCE: Dr Tan Toh Lick, Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, 100 Bukit Timah Road, Singapore 229899, Singapore. Email: tan.toh.lick@kkh.com.sg |
References
- WHO recommendations for Induction of labour. Geneva, World Health Organization, 2011.
- National Collaborating Centre for Women’s and Children’s Health. Induction of labour. London: RCOG Press; 2008.
- Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M. Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2012 Mar 14;3.
- Vaknin Z, Kurzweil Y, Sherman D. Foley catheter balloon vs locally applied prostaglandins for cervical ripening and labor induction: a systematic review and metaanalysis. 11. Am J Obstet Gynecol. 2010 Nov; 203(5): 418-29.
- Rey E, Boulet LP. Asthma in pregnancy. BMJ 2007; 334: 582–5.
- Kwon HL, Belanger K, Bracken MB. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol 2003; 13: 317–24.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




