Combined Botulinum Toxin Injections and Phenol Nerve / Motor Point Blocks to Manage Multifocal Spasticity in Adults
Fahim Anwar & Shruthikaa Ramanathan
Cite this article as: BJMP 2017;10(1):a1002
|
|
Abstract Objectives: To highlight the importance of combining phenol and botulinum toxin in the treatment of spasticity in adult patients resulting from upper motor neuron lesion. Abbreviations: INR - International Normalised Ratio |
Introduction
Spasticity was first described by Lance1 in 1980, and according to him it was described as; a motor disorder characterised by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex, as one component of the upper motor neuron syndrome. Spasticity can be a consequence of many neurological conditions including traumatic brain injury, spinal cord injury, stroke and multiple sclerosis. The annual incidence of spasticity in the lower limb following a stroke, traumatic brain injury and spinal cord injury is estimated to be 30 to 485 per 100,000, 100-235 per 100,000 and 0.2 to 8 per 100,000 respectively2. Spasticity is characterised by muscle overactivity and can lead to permanent changes in the muscle fibres leading to muscle contractures. Contractures can be very painful and may interfere with seating, posture, mobility and activities of daily living, thus increasing the care cost significantly.
Phenol has been used peripherally and intrathecally for the treatment of spasticity for many years. The botulinum toxin became available in the last decade for treatment of spasticity. Its use has increased since then, and this has led to a decline in the use of phenol. It is still being used in patients who are sensitive to botulinum toxins or have developed antibodies to them. Phenol is both neurolytic and anaesthetic in nature3. The anaesthetic effect of phenol can be seen immediately after the injection where the patient reports an immediate effect. The neurolytic effect takes at least two weeks, and therefore patients should be educated not to expect any significant change in the spasticity before two to four weeks. Phenol can also be used in combination with botulinum toxin to treat multifocal spasticity where the maximum dose of botulinum exceeds the recommended safe dose. This allows several groups of muscles to be treated in a single setting3.
The lethal dosage of phenol has been reported to be greater than eight grams4. Phenol in aqueous solution is preferred for peripheral nerve and motor point blocks and is available in 5, 6 and 7% concentration. Injecting botulinum toxins is quite different from performing nerve and motor point blocks. Phenol nerve and motor point blocks take a longer duration of time to perform as compared to botulinum toxins. For motor point blocks, a nerve stimulator with a surface electrode is needed to localise the motor points on the muscles. In the present study, we highlight the importance of management of spasticity in adults with a combination of botulinum toxin and phenol nerve /motor point blocks. A case series of patients who underwent combined phenol and botulinum toxin is presented, describing the diagnosis, number and location of muscles injected, types of phenol nerve and motor point blocks and any complications encountered.
Methods
This is a retrospective study conducted at the Rehabilitation Medicine Department of the University Hospital in Cambridge UK. The study period included from December 2014 to January 2017. The patients were identified from the spasticity clinic database. All patients were assessed in the spasticity clinic, and a plan to inject the botulinum toxin along with phenol nerve block/motor point block agreed with the patient. The patients who decided to have the procedure were appointed to a clinic to perform the agreed injections and blocks. If the patients were on anticoagulants (warfarin, dalteparin or clopidogrel), they were advised to stop the anticoagulation 3 days before the procedure. International Normalised Ratio (INR) was checked before the procedure. The usual dose of anticoagulation was started after the procedure.
Patients were consented and placed on a plinth. Botulinum toxin type A only was used in our study. It was diluted with normal saline, and the muscles were injected either using the surface anatomy or electrical stimulation. Each muscle was either injected at one to two sites, depending on the size of the individual muscle.
Phenol nerve blocks and motor point blocks were performed according to the techniques described by Roy3 and Gaid5. Aqueous phenol 5% (phenol in water) was used for all the procedures. The nerves were identified using a nerve stimulator with a surface electrode using 2mA current (Figure 1). The skin was infiltrated with 1% lignocaine, and the nerve was approached with a stimulator needle. The nerve was then ablated with 5% phenol under stimulation guidance. The dose of the phenol was titrated while the nerve was being stimulated. The motor points were located similarly with the help of a surface electrode and marked before ablation with 1 to 2 ml of 5% phenol. The amount of botulinum toxin and phenol was recorded. All patients were reviewed in 6 weeks’ time for any complications.
Figure 1: Nerve Stimulator with surface electrode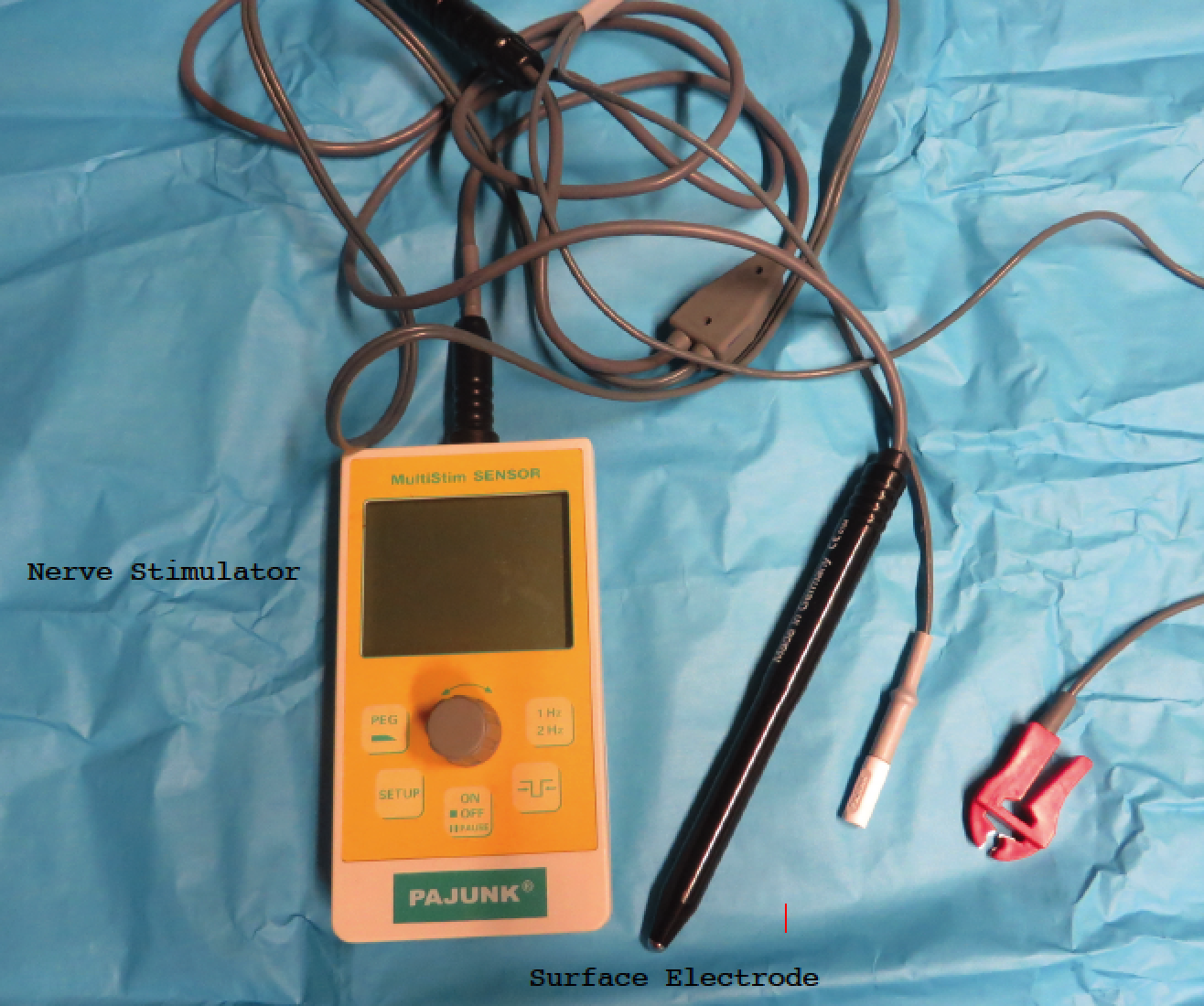
Results
Between December 2014 to January 2017, we treated 29 patients with spasticity caused by different neurological conditions with a combination of aqueous phenol and botulinum toxin injections. There were 15 males and 14 females with an age range of 18 to 80 years and a mean age of 49.3 years. The most common diagnosis was multiple sclerosis followed by stroke (Figure 2). A total of 40 phenol nerve or motor point blocks were performed in 29 patients. Nineteen patients (65.5%) received phenol blocks once, 9 (31%) twice and only 1 patient (3.4%) had the phenol block done three times. Where the phenol blocks were repeated, the mean duration between the phenol injection was 14.1 months (range 6-23 months). The procedure was bilateral in 16 (55.2%) and unilateral in 13 (44.8%). The local anaesthetic (trial block) was performed in 6 (20.6%) patients who were ambulatory before the phenol block.
Figure 2: Frequency of Diagnosis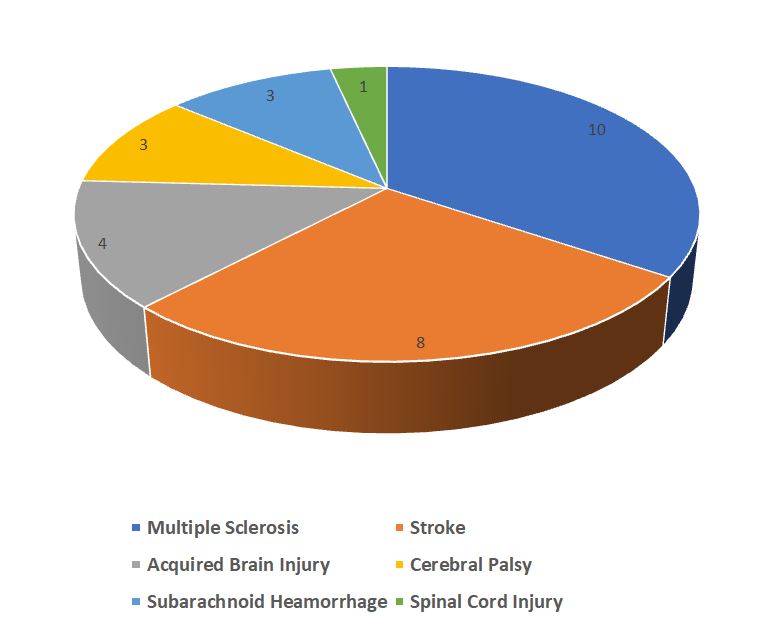
Obturator nerve block was the most common phenol procedure performed (44.8%), followed by posterior tibial nerve block (37.9%). Two (6.9%) patients had both obturator nerve blocks and posterior tibial nerve blocks, whereas 1(3.4%) patient had hamstring motor point blocks, 1(3.4%) patient had gastrocnemius motor point blocks. One patient (3.4%) had bilateral obturator nerve blocks, posterior tibial nerve blocks and rectus femoris motor point blocks (Figure 3).
Figure 3: Frequency of Phenol Nerve/Motor Point Blocks
Botulinum toxin was also injected into various muscles in all 29 patients. The botulinum was repeated every 4 to 6 months in the same muscles. Botulinum toxins were injected bilaterally in 12 (41.4%) and unilaterally in 17 (63.6%) patients. The most common muscles injected with botulinum toxin were hamstrings (44.8%) followed by finger flexors (13.8%). The frequency of botulinum toxins injections is shown in Figure 4.
Figure 4: Muscles Injected with Botulinum Toxins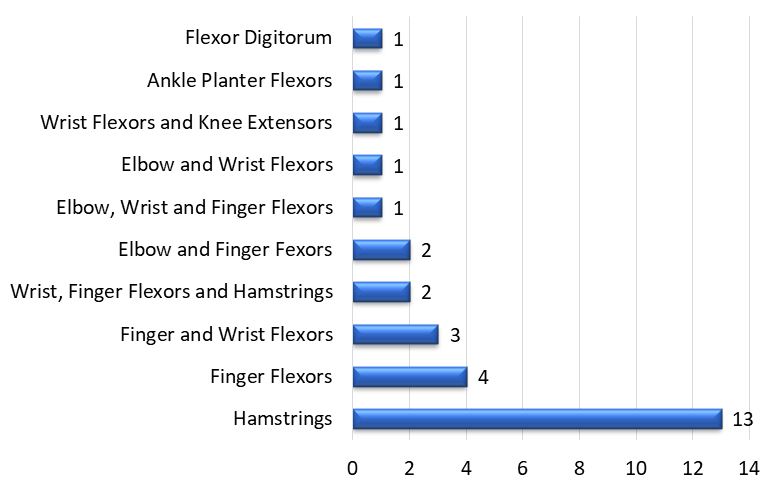
The most common combination in our series was obturator nerve block and hamstring botulinum toxin injections (34.4%). The combination of posterior tibial nerve block with hamstring botulinum toxins was used in 3 (10.3%), and 2 (6.8%) patients received posterior tibial nerve block with finger flexor botulinum toxin injections. The combination of phenol and botulinum toxin injection is shown in Table 1. There were no complications noted following both phenol as well as botulinum toxin injections.
Table 1: Combination of Phenol and Botulinum Toxins used
|
Phenol Nerve/Motor Point Blocks |
|||||||
| Obturator Nerve Block | Posterior Tibial Nerve Block | Obturator and Posterior Tibial Nerve Block | Hamstrings Motor Point Blocks | Gastrocnemius Motor Point Blocks | Obturator, Posterior Tibial Nerve Block and Rectus Femoris Motor Point Block | ||
|
Muscles Injected with Botulinum |
Hamstrings | 10 | 3 | 0 | 0 | 0 | 0 |
| Finger Flexors | 0 | 2 | 1 | 0 | 0 | 0 | |
| Finger and Wrist Flexors | 0 | 2 | 0 | 1 | 0 | 0 | |
| Wrist, Finger Flexors and Hamstrings | 1 | 0 | 1 | 0 | 0 | 0 | |
| Elbow and Finger Flexors | 0 | 1 | 0 | 0 | 1 | 0 | |
| Elbow, Wrist and Finger Flexors | 0 | 1 | 0 | 0 | 0 | 0 | |
| Elbow and Wrist Flexors | 0 | 1 | 0 | 0 | 0 | 0 | |
| Wrist Flexors and Knee Extensors | 1 | 0 | 0 | 0 | 0 | 0 | |
| Ankle Planter Flexors | 1 | 0 | 0 | 0 | 0 | 0 | |
| Flexor Digitorum | 0 | 1 | 0 | 0 | 0 | 0 | |
Discussion
Perineural injection of aqueous phenol (3 to 7%) can reduce spasticity by blocking the nerve signals to the group of muscles supplied by the nerve. Phenol produces an initial local anaesthetic effect which is followed by neurolysis caused by protein coagulation and inflammation6. The neurolysis leaves the nerve with about 25% less function than before but does not disadvantage people with little or no residual function, as a mild progressive denervation can be beneficial in reducing spasticity6. Khalili et al7first described the technique of phenol nerve blocks and also suggested that the re-growth of most axons is seen with preservation of gamma motor neurons. This means that phenol reduces spasticity without reducing the strength of the muscle significantly.
The use of combining phenol with botulinum toxins injections has been documented in children with cerebral palsy and central nervous degenerative diseases8. To date, there are no studies in the literature showing the use of combined phenol and botulinum toxins in the treatment of spasticity in adults. The combination of phenol with botulinum toxin helps to treat multifocal spasticity allowing more spastic areas to be treated. The most frequent pattern used in Gooch et al8 study was obturator nerve block and gastrocnemius botulinum toxin injections. In our study, the most common combination was obturator nerve block and hamstring botulinum toxin injections. The possible explanation for this variance is that the majority of our study population suffered from multiple sclerosis and hamstring with hip adductor spasticity is a very common pattern.
The mechanism of action of phenol is different from botulinum toxins. However, the reduction in spasticity with phenol and botulinum toxins is comparable. Manca et al9 compared botulinum toxins and phenol nerve blocks to reduce ankle clonus in spastic paresis and concluded that both patient groups showed significant clonus reduction over time with the phenol group effect greater than the botulinum toxins group. They also suggested that the two drugs have a different mechanism of action with phenol reducing the excitability of the alpha motor neuron. A randomised double-blind trial by Kirazli et10 al compared the effects of botulinum toxins Type A and phenol on post-stroke ankle plantar flexor and invertor spasticity. There was a significant change in Ashworth scores at week 2 and 4 in the group who received botulinum toxins but there was no significant difference between the two groups at week 8 and 1210. Similarly, the decrease in clonus duration (detected by electromyography) was significant in both groups. However, the group that received botulinum toxins showed significant change at week 2 and 4 compared to phenol group. The reason for this may be the delayed onset of action of phenol as compared to botulinum toxins. Burkel et al6 studied the effects of phenol into the peripheral nerves of rats and showed that Wallerian degeneration of the nerves occurs before healing by fibrosis that starts after about 4-6 months following phenol injections. Their study also concluded that following phenol the nerves are left with 25% less function than before and this does not disadvantage the people with little or no residual function6.
There is always a risk of deteriorating the mobility or function due to weakness caused by the phenol nerve block. It is our usual practice to perform a local anaesthetic block (trial block) before injecting the phenol in all ambulatory patients or patients who are using spasticity functionally to their advantage. In our series, 20.6% of patients underwent local anaesthetic block before proceeding to the phenol block. There were no adverse effects noted following the local anaesthetic block, and all six patients chose to have the phenol blocks. A recent study by McCrea et al11 looked at the effects of phenol on position and velocity components of spasticity in addition to strength in post-stroke elbow flexor spasticity. The study concluded that phenol paradoxically improved muscle strength in addition to reducing hypertonia11.
In our series, we used phenol mainly for lower limb muscles and botulinum toxins for both the lower and upper limb muscles. For smaller muscles of the upper limb, it is difficult, but not impossible, to find the motor points. The technique for upper limb phenol blocks has been well described in literature3. However, when combining the botulinum toxins with phenol, we find it useful to prefer the phenol block for the lower limb muscles. Gooch et al8 also injected larger proximal muscles with phenol, and smaller distal and deeper muscles with botulinum toxins. In our series, the maximum dose of botulinum toxins used was 1000 units of Dysport and the maximum dose of phenol used was 20 ml of 5% aqueous phenol.
Conclusion
The combination of botulinum toxin with phenol injections is effective in treating multi-focal spasticity in clinical settings. The advantage of using phenol in combination with botulinum toxins is cost-reduction and the flexibility of managing various muscle groups at the same time. Further studies are needed to evaluate the long-term cost-effectiveness and complications of combining phenol and botulinum toxins, especially after repeated injections.
|
Acknowledgements NONE Competing Interests None declared Author Details FAHIM ANWAR, MBBS, MRCS, FRCP, FEBPRM, Cambridge University Hospital Nhs Foundation Trust SHRUTHIKAA RAMANATHAN, MBBS, MRCP, Cambridge University Hospital Nhs Foundation Trust CORRESPONDENCE: FAHIM ANWAR, Box 248, Addenbrooke's Hospital, Cambridge, United Kingdom Email: fanwar@nhs.net |
References
- Feldman RG, Young RR, Koella WP, Spasticity, disordered motor control. Miani, FL: Symposia Specialist; Chicago; 1980. 485-494p.
- Martin A, Abogunrin S, Kurth H. Epidemiological, humanistic, and economic burden of illness of lower limb spasticity in adults: a systematic review. Neuropsychiatric Disease and Treatment 2014; 23(10):111-22.
- Roy C. Phenol Block for Upper Limb Spasticity. ACNR 2012; 12(5): 34-36.
- Gracies JM, Elovic E, McGuire J, et al. Traditional pharmacological treatments for spasticity. Part I: Local treatments. Muscle Nerve Suppl. 1997;6:S61–91.
- Gaid M. Phenol Nerve Block for the Management of Lower Limb Spasticity. ACNR 2012;12(13):1–3.
- Burkel WE, McPhee M. Effect of phenol injection into peripheral nerve of rat: electron microscope studies. Archives of physical medicine and Rehabilitation 1970 ;51(7):391–7.
- Khalili AA, Harmel MH, Forster S, Benton JG. Management of Spasticity by Selective Peripheral Nerve Block with Dilute Phenol Solutions in Clinical Rehabilitation. YAPMR. W.B. Saunders Ltd; 1964; 45:513–9.
- Gooch JL, Patton CP. Combining botulinum toxin and phenol to manage spasticity in children. Archives of Physical Medicine and Rehabilitation 2004;85(7):1121–4.
- Manca M, Merlo A, Ferraresi G, et al. Botulinum toxin type A versus phenol. A clinical and neurophysiological study in the treatment of ankle clonus. Eur J Phys Rehabil Med 2010;46(1):11–8.
- Kirazli Y, On AY, Kismali B, et al. Comparison of Phenol Block and Botulinus Toxin Type A in the Treatment of Spastic Foot after Stroke: A Randomized, Double-Blind Trial. American Journal of Physical Medicine & Rehabilitation 1998;77(6):510.
- McCrea PH, Eng JJ, Willms R. Phenol Reduces Hypertonia and Enhances Strength: A Longitudinal Case Study. Neurorehabilitation and Neural Repair 2004;18(2):112–6.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




