David Cash, Jens Bayer, Karl Logan and James Wimhurst
Abstract
INTRODUCTION The Exeter Trauma Stem (ETS) is a new monoblock unipolar prosthesis with no independent published series using this implant. This study prospectively evaluates the first 50 ETS hemiarthroplasties performed as a primary treatment for fractured neck of femur at Norfolk and Norwich University Hospital.
METHODS Patient demographics and operative details were recorded from the patient notes. Radiographic evaluation involved the Barrack cementation grading system, Dorr’s criteria and leg length measurement. All patients were sent an Oxford Hip Score questionnaire between two and four months postoperatively with 100% response rate.
RESULTS Two thirds of cement mantles were Barrack grade A and B. Twenty-eight patients had lengthening of the operated limb with a mean of 12mm (5-30) including one irreducible prosthesis. Further complications included three deaths and one deep infection. The average Oxford Hip Score was 27.2.
DISCUSSION Patient demographics were similar to previous studies. There was no statistical difference between the cement mantles and those of another published study using the Exeter stem. The major difficulty evident from this study was correct positioning of the prosthesis with regards to leg-length. Post-operative hip scores were similar to other studies as was the mortality rate.
CONCLUSION - Post-operative functional and radiographic scoring of the ETS prosthesis were encouraging but care is needed with regards to correct positioning of this prosthesis to attain equal leg lengths. Subsequent to the results of this study, a trialling system has been added to the instrumentation which the authors recommend in conjunction with pre-operative templating. Keywords: Exeter Trauma Stem, Cemented hemiarthroplasty, Hip fractures, Leg length inequality, Barrack Grading, Oxford Hip Score.
|
INTRODUCTION
The Western world is experiencing a rapid increase in the incidence of femoral neck fractures, from 50000 fractures in 1990 to a projected 120000 in 20151 as the age of the population increases. Hip fractures account for approximately 20 percent of orthopaedic bed occupancies in Britain at a total cost of up to £25000 per patient1.Around half of these fractures are intracapsular in nature of which two thirds are displaced.
The ideal surgical treatment for displaced intracapsular femoral neck fractures remains controversial with studies indicating a lack of consensus among treatment centres2,3. Options include reduction with internal fixation, cemented or cementless hemi-arthroplasty and total hip replacement. Internal fixation is less traumatic than arthroplasty but has a higher re-operation rate4,5 whilst cemented femoral prostheses are associated with a lower rate of revision compared to cementless implants. In addition there are statistically significant improvements in pain scores, walking ability, use of walking aids and activities of daily living within the cemented group6,7. The cementation process may however be associated with increased morbidity due to fat embolisation and increased length of operation8.
Treatment planning for intracapsular fractures, therefore, needs to take into account the patient’s medical fitness and activity level as well as the cost-effectiveness of the procedure.
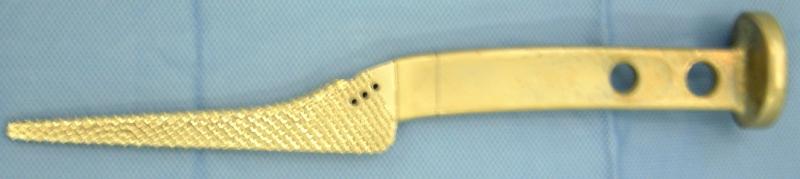
Figure 1: Exeter Trauma Stem (ETS) Implant
The Exeter Trauma Stem is a new monoblock unipolar implant using an intermediate size 1.5, forty millimetre offset Exeter stem with a large head sized to match the patient’s anatomy (Figure 1, 2).
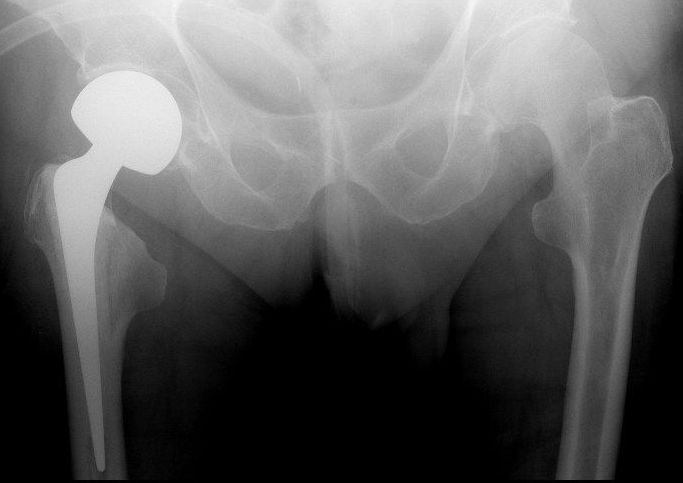
Figure 2: X-ray of ETS with correct length. Neck cut has been made 1cm above lesser trochanter with shoulder of prosthesis sunk below greater trochanter to ensure equal leg length
As yet there are no independent published series of the results of using this implant. Purported advantages of the ETS include the use of a tried and tested polished, tapered stainless steel stem with which many primary hip surgeons are familiar, ease of ‘cement-in-cement’ revision to a total hip replacement should the patient develop acetabular erosion and the relatively low cost of £240 compared to many contemporary cemented implants.
This study prospectively evaluates the first 50 ETS hemiarthroplasties performed at the Norfolk and Norwich University Hospital, UK over a six month period providing an indication of early outcomes and complications involved with the use of this prosthesis.
METHOD
Patients presenting to our unit with a displaced intracapsular femoral neck fracture who were sufficiently active to get out of their home independently, had an ASA grade of 1 or 2 and were not significantly cognitively impaired were treated with a cemented ETS prosthesis. In addition, patients with displaced intracapsular fractures associated with significant comminution of the medial femoral neck precluding the use of our standard calcar-bearing Austin Moore (Stryker Howmedica Osteonics Ltd) hemiarthroplasty were also treated with an ETS regardless of functional capability and medical condition.
The first fifty patients who underwent ETS hemiarthroplasty as a primary treatment for fractured neck of femur were included in the study. Four patients were excluded. Two of these patients had an ETS performed due to failure of cancellous screw fixation and two as part of a two stage revision for infected uncemented prosthesis.
All fifty procedures were performed with the patient in the lateral position via the modified lateral approach with the glutei incised at the musculotendinous junction. Cefuroxime was given on induction in each instance followed by two post operative doses at eight and sixteen hours after the procedure. Patients were scored by the hospital protocol for risk of thrombosis and were administered aspirin or subcutaneous low-molecular weight heparin as appropriate. All drains were removed between twenty-four and forty-eight hours and patients were mobilised within one day of operation as pain allowed.
Patient demographics and operative details were gathered both from the patients’ notes and from the ORSOS computerised theatre system.
Radiographic evaluation involved the Barrack9 cementation grading system, Dorr’s criteria10,11 including varus/valgus alignment of the prosthesis and leg length measurement.. Measurements of length and varus/valgus were performed using the PACS (GE Medical Systems 2005) digital imaging system by two orthopaedic registrars independent of one another.
Finally all fifty patients were sent an Oxford Hip Score12 at between two and four months postoperatively. Three patients died before the questionnaires were sent and of the remaining forty seven, there was a 98% response rate with 44 questionnaires completed solely by the patient and a further two completed with the aid of a carer.
RESULTS
1. Patient Demographics and operative details
Of the fifty patients in the study, thirty six were female and fourteen male. The mean age was 78 (range 38 to 99). Forty four ETS hemiarthroplasties were performed due to patient fitness and activity levels (Type 1 patients) with six undertaken in frail patients due to fracture extension into the calcar (Type 2). All type 1 patients were ASA grade 1 or 2 with all type 2 patients ASA grade 2-4. All type 1 patients had a mini-mental test score of 10/10 with type 2 patients ranging from 0-7.
The mean delay to surgery was 26 hours (9-58). Eight procedures were performed by consultants, thirty eight by registrars (training years three to six) and four by the trauma fellow under supervision by a senior. The mean operative time was sixty four minutes and the mean haemoglobin drop was 2.6 g/dl3 . Seven patients required post operative transfusion of either two or three units of packed cells.
Thirty four of the patients mobilised unaided pre-injury with eight using one stick, four using two sticks and four using a frame. Using the four categories above, the average drop in mobility from injury to discharge was 1.6 levels.
The average hospital stay was 8.6 days (range 5-69) with thirty five patients discharged to their own house, four to their own residential home and eleven to a rehabilitation ward.
2. Radiographic Evaluation
The cement mantle was firstly evaluated using Barrack’s grading:-
grade A: medullary canal completely filled w/ cement (white out).
grade B: a slight radiolucency exists at the bone cement interface.
grade C: a radiolucency of more than 50% at the bone cement interface.
grade D: radiolucency involving more than 100% of the interface between bone and cement in any projection, including absence of cement distal to the stem tip
Post-operative radiographic evaluation according to this system showed that 54% of cement mantles were Barrack grade B (27 cases) with the majority of the remainder grade C (12 cases) and grade A (eight cases). Two were graded as D.
Dorr’s criteria were employed firstly to assess whether there was an adequate cement thickness of 3mm in Gruen zones 3 and 7 and of one centimetre distal to the tip of the prosthesis. Thirty-four prosthesis scored 3/3, nine scored two, four scored one and two scored none.
Dorr’s criteria also assess position of the prosthesis using the AP radiograph. Ten prostheses were placed in a neutral position related to the femoral shaft. Seven were placed in 1-2 degrees of varus, twenty-seven were placed in 1-2 degrees of valgus and five were placed in 3-6 degrees of valgus.
There were equal leg length measurements in nineteen patients post-operatively with two patients left 5-10mm short on the operated side. Twenty-eight patients were left long with a mean lengthening of 12mm (5-30) and of these five were left between 20 and 30mm long one of which was irreducible and needed to be revised on the table.
3. Post-operative Scoring
The Oxford Hip Score contains 6 questions relating to pain and six relating to function and mobility which are scored 1 point for the best outcome and five for the poorest (Score 12-60). The average pain score was 12.0 and the average functional score was 15.2 giving an overall score of 27.2. The type 1 patients fared better with an average score of 25.3, the average score for type 2 patients was 44.3
4. Complications
The one immediate complication was the need for an on-table revision due to an irreducible prosthesis.
There was one superficial wound infection requiring antibiotic therapy and one early deep infection requiring open washout in theatre which resolved the infection in combination with antibiotic therapy.
There were three deaths (one CVA, one MI and one from pneumonia) all of which occurred between 30-90 days from the operative procedure.
DISCUSSION
The cohort of patients included in this study was similar to other studies with regards to male:female ratio, age and cognitive function4,5. The patients also experienced a delay to surgery and length of operation similar to previous studies4,7. The length of inpatient stay, however, was markedly better at 8.6 days compared to approximately fourteen to twenty-one days cited in the literature13,14.
The length of operation, post-operative mobility and transfusion requirements were also similar to studies evaluating hemiarthroplasty outcomes4,5.
Post-operative radiographic evaluation showed greater than 50% of cement mantles were Barrack grade B with the majority of the remainder grade C (24%) and A (16%). There was no statistical difference between our findings and those of an 8-12 year study of the Exeter stem in total hip replacement15. The two Barrack D grade cement mantles were in patients who became unwell intra-operatively and the decision was taken not to pressurise during cementation.
Figure 3: Original ETS broach with squared off handle, not allowing intra-operative trialling
The major difficulty evident from this study is the correct positioning of the ETS prosthesis with regards to restoration of accurate leg length which the authors believe was due to two reasons. Firstly, the original set for the Exeter Trauma Stem comes with one femoral broach (Fig 3) which does not allow trial reduction. Therefore positioning of the prosthesis required intra-operative estimation of the correct leg length which can be difficult with hip fractures as the leg length is abnormal at the commencement of surgery. Therefore the centre of rotation of the femoral head on the injured side was approximated by comparison with the contralateral side on the pelvic AP radiograph and referenced against the level of the greater trochanter during the procedure.
Secondly, because the large monoblock head of the ETS is matched to the patient’s own femoral head anatomy, the diameter of the ETS head is generally around 15-30mm wider than the 28mm heads commonly used with the Exeter stem in elective hip arthroplasty. Therefore care must be taken to sink the stem by a corresponding amount if a similar neck cut is used or the femoral neck osteotomy should be made at a more distal level. This often involves positioning the shoulder of the ETS stem below the level of the greater trochanter. This can mislead surgeons who are familiar with the Exeter stem as placing the ETS stem in a similar position to that employed with smaller head elective arthroplasty results in limb lengthening. Figure 4 shows a leg length discrepancy of 15mm despite a low neck cut as the stem has not been sunk sufficiently. This led to 56% of patients being left with true lengthening of the operated limb and one prosthesis irreducible. It is difficult to assess whether this is a common problem in the literature with other hemiarthroplasties used for femoral neck fractures as none of the comparable studies comment on clinical or radiographic assessment of leg length.
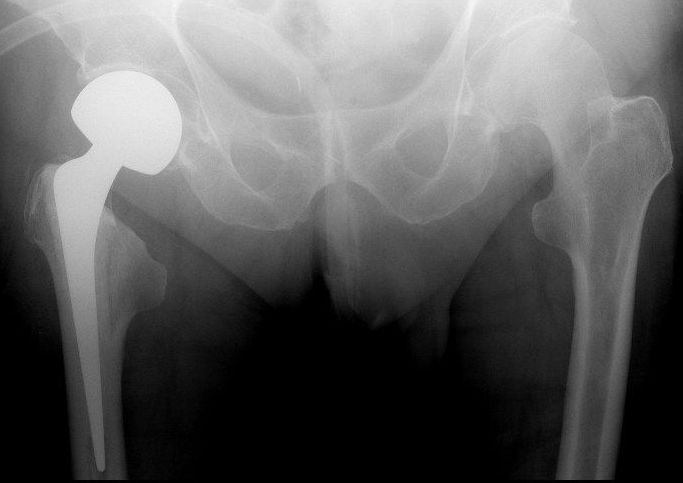
Figure 4: X-ray of ETS with limb lengthening. Although the neck cut has been made relatively low in relation to the lesser trochanter, the shoulder of the prosthesis slopes marginally above the greater trochanter, inadvertently lengthening the operated limb.
One major advantage to the tapered Exeter stem is the ease with which conversion to a total hip replacement can be performed using an in-cement technique16. Many of the patients included in this study were below the age of 70 and a proportion could be expected to outlive the prosthesis especially with regards to acetabular erosion4. Whilst none of this cohort has required revision for loosening, the irreducible Exeter implant was revised on-table using this technique without further complication.
Post operative Oxford Hip Scores were encouraging with no difference between our mean score of 27.2 and other studies evaluating both cemented hemiarthroplasty and total hip replacement following femoral neck fracture12,17,18.
The mortality rate was 6% six to twelve months post surgery with all three deaths more than one month post surgery and apparently unrelated to the surgery itself. Overall mortality rates following neck of femur fracture are approximately thirty percent at one year however studies specifically looking at outcomes following cemented hemiarthroplasty in the fit and active patient have found mortality rates similar to this study5,19.
Costing around £240, the ETS is a relatively cheap prosthesis in comparison to cemented bipolar prosthesis depite the additional expense of a cement restrictor, bone cement, cement gun and cement pressurisers.
In conclusion, the Exeter Trauma Stem (ETS) is an effective method of treating displaced intracapsular neck of femur fractures with encouraging post-operative functional, pain and radiographic scoring outcomes. The message highlighted by this study is that additional care is needed with regards to the correct positioning of the prosthesis to ensure the restoration of limb length. Subsequent to discussion with the Stryker representative regarding the results of this study, a second generation trialling system has been added to the set with a modular broach. The authors suggest that not only should these modular broaches be used, but also accurate pre-operative planning is needed to ensure equal leg lengths post-operatively.
Competing Interests
Author would like to state that none of the authors involved with this paper have any financial or personal relationship with Stryker or any other companies that could inappropriately influence this study.
Author Details
DAVID CASH, JENS BAYER, KARL LOGAN: Specialist Registrars, Orthopaedic Department, Norfolk and Norwich Hospital
JAMES WIMHURST, Consultant orthopaedic Surgeon, Orthopaedic Department, Norfolk and Norwich Hospital
CORRESPONDENCE: Mr. D Cash, Specialist Registrar, Orthopaedic Dept, Addenbrooke’s Hospital, Long Road, Cambridge CB2 0QH
Email: davecash@doctors.org.uk |
References
1. Parrott S : The economic cost of hip fracture in the UK (2000) www.dti.gov.uk/files/file21463.pdf2. Crossman PT, Khan RJK, MacDowell A, Gardner AC, Reddy NS, Keene GS A survey of the treatment of displaced intracapsular femoral neck fractures in the UK. Injury, 33(2002): 383-3863. Anderson GH, Harper WM, Gregg PJ: Management of the intracapsular fractures of the proximal femur in 1990 : a cause for concern? J Bone Joint Surg (Br) 73B(Suppl 1) (1991) : 734. Parker MJ, Khan RJK, Crawford J, Pryor GA: Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. J Bone Joint Surg (Br), 84(8) (2002): 1150-55. Davison JNS, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ: Treatment for displaced intracapsular fracture of the proximal femur. J Bone Joint Surg (Br) 83 (2001) : 206-16. Khan RJK, MacDowell A, Crossman PT, Keene GS: Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip – a systematic review. Injury 33 (2002) : 13-177. Keating JF, Grant A, Masson M, Scott NW and Forbes JF: Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am, 88(2) (2006): 249-60,8. Parker MJ: The management of intracapsular fractures of the proximal femur. J Bone Joint Surg (Br) 82 (2000) : 937-419. Barrack RL, Mulroy, RD Jr and Harris WH: Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br, 74(3) (1992.): 385-910. Dorr LD, Luckett M and Conaty JP: Total hip arthroplasties in patients younger than 45 years. A nine to ten-year follow-up study. Clin Orthop Relat Res, (260) (1990.): 215-911. Dorr LD, Takei GK and Conaty JP: Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am, 65(4) (1983): 474-912. Dawson J, Fitzpatrick R, Carr A, and Murray D: Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br, 78(2) (1996.): 185-9013. Department of Health. Hospital episode statistics, England: Financial year 1993-1994; volume 1. London: HMSO, 1994.14. Hay D, Parker MJ: Hip fracture in the immobile patient. J Bone Joint Surg (Br) 85 (2003) : 1037-915. Williams HDW, Browne G, Gie GA, Ling RSM, Timperley AJ, Wendover NA: The Exeter universal cemented femoral component at eight to twelve years J Bone Joint Surg (Br) 84 (2002) 324-3416. W W Duncan, M J W Hubble, A J Timperley and G A Gie: Cement in cement femoral revision with the Exeter hip. J Bone Joint Surg (Br) 88 (Suppl 2) (2006) : 23917. Mishra V, Thomas G, Sibley TF: Results of displaced subcapital fractures treated by primary total hip replacement. Injury 35(2) (2004) :157-60.18. Wazir NN, Mukundala VV, Choon DSK: Early results of prosthetic hip replacement for femoral neck fractures in active elderly patients. J Orthop Surg 14 (2006) 43-619. Keating JF, Grant A, Massom M, Scott NW, Forbes JF: Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess 9 (2005) 1-65

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.