A feasibility study to establish a Deliberate Self-harm Register in a state hospital in southern India.
Rajgopal Rajendra, Murali Krishna, Sumanth Majgi, Narendra Heggere, Catherine Robinson and Rob Poole
Cite this article as: BJMP 2015;8(1):a807
|
|
Abstract Background: Deliberate self harm (DSH) registers are the first step towards understanding self-harm in developing countries. Abbreviations: DSH : Deliberate Self Harm, ICD: International Classification of disorders |
BACKGROUND
Suicide and deliberate self-harm (DSH) have been recognised as major public health problems in India for some time, but there are significant obstructions to effective intervention including difficulties in following Western models to understand these behaviours.1, 2, 3
The World Health Organisation (WHO) recognises suicide as one of the three leading causes of death in young adults globally.4 The greatest burden of suicide is now in low- and middle-income countries like India where annual suicide rates are 10-11 per 100,000.5, 6, 7 India is second only to China in the absolute number of annual deaths by suicide.5 The number of individuals who die by suicide each year in India alone is more than the total number of suicides in the four top ranked European countries combined.3, 5, 8
DSH, defined as intentional self-poisoning or self-injury, is a closely related public health problem.9WHO estimates that for every suicide there are at least 10-20 DSH acts.10 If this estimated proportion, based on Western research, is also true in India then there are 1-2 million DSH acts in India each year.
Official data for 2005 suggest that 19.6% (n=22,327) of India's 113,914 officially recorded suicides were self-poisonings with pesticides7 (predominately organophosphates, which are freely available and widely used in agriculture). The official suicide rate for India, 10.3 per 100,000 in 2005,7 is thought to be an under-estimate.3, 11 Studies from several regions suggest that India's suicide rates may be as high as 40 per 100,000 and that 30% or more of these deaths are due to pesticide self-poisoning.11 The studies reporting the highest suicide rates within India are from Tamil Nadu (>60 per 100,000 – three times higher than the official figure for the state).12, 13, 14, 15 Whilst some of the discrepancies between official statistics and findings in local studies may be due to urban-rural differences in the incidence of suicide, data collated by the Indian police suggest that around 90% of suicides in India occur in non-urban areas.7, 11, 15 Extrapolating from these figures, it is conservatively estimated that there may be up to 420,000 suicides per annum in India (126,000 from pesticide self-poisoning).
India's centrally collated self-harm and suicide data are unreliable owing to a number of factors. Death registration processes are below Western standards. Only about 25% of deaths are registered and only about 10% are medically certified.16, 17 Attempted suicide is a crime in India.18 Survivors are interviewed by the police. Fear of legal and social consequences following an act of self-harm probably influence willingness to acknowledge DSH and preparedness to seek medical intervention.
India contributes almost 20% to the world's population, and suicides rates are increasing particularly amongst the young.11, 19 Obtaining reliable and nationally representative data on DSH rates in India should be a priority for health-funding agencies over the next decade. In order to reduce fatalities following self-harm, information and investment are needed to improve quality, affordability and accessibility of health care close to the affected communities.20
If, as seems likely, self-harm (especially pesticide poisoning) occurs predominantly in rural areas of India,11 Western models of data collection and intervention aimed at reducing pesticide poisoning (which is predominately accidental in developed economies) are likely to require significant modification to be reliable and effective. The WHO's global suicide prevention strategy is largely based on findings from research and models of suicide prevention developed in the West.21 Health care resources in rural areas of India are thinly spread, and are often rudimentary compared to those in the West. There is an urgent need for research in low- and middle-income communities – particularly in rural areas of India – to provide the evidence base to underpin public health strategies for preventing pesticide suicides in these countries.
The establishment of DSH registers is a first step towards the systematic collection of data in relation to self-harm, both for epidemiological purposes and to understand pesticide self-poisoning at an individual level. If DSH registers can be shown to generate reliable information in India, in due course it may be possible to identify the factors that put individuals at risk of behaving in this way, and create relevant evidence-based policies to develop interventions for reducing mortality and morbidity associated with DSH (particularly pesticide poisoning).
This paper explores the feasibility of setting up a DSH register in a resource-poor large State hospital in south India, where rates of suicide and DSH are high.
METHODS
Setting
This study was carried out at Mysore Medical College and Research Institution (MMCRI), a State-run hospital in Mysore, southern India. The hospital serves a catchment area of 1,500,000 population and 135 primary health centres. The hospital has most specialities, with 1050 beds and a 10-bedded intensive care unit. 800-1000 patients attend the hospital outpatient department daily. Daily attendance to the casualty department for the purpose of medico-legal registration (which includes self-harm) is between 110 and 130. All other presentations including emergencies are managed through respective speciality outpatient departments.
Figure 1. Care Pathway for deliberate self-harm (DSH) at Mysore Medical College and Research Institution (MMCRI)
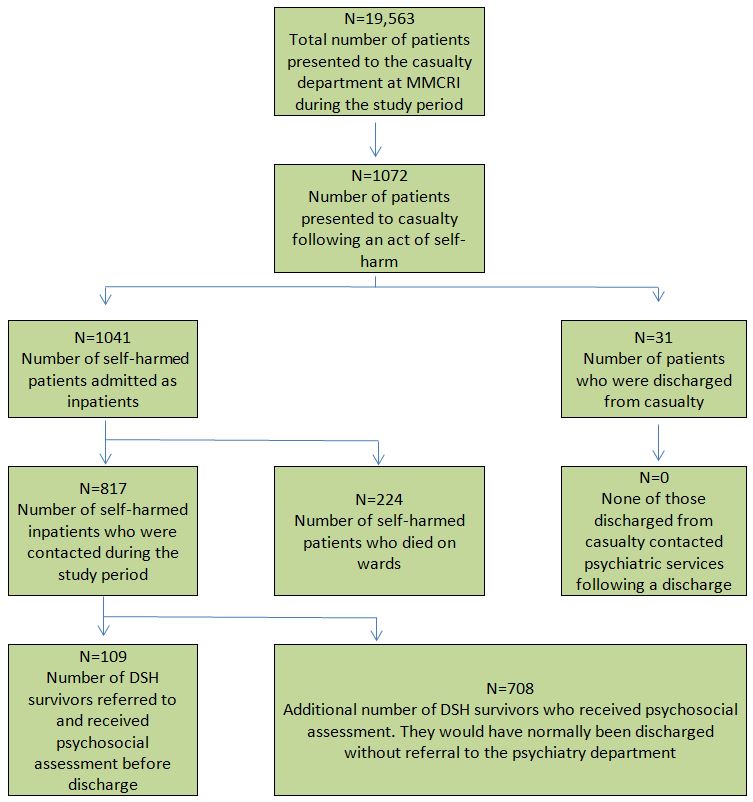
Setting up of the register
The flow diagram (Fig. 1) illustrates the care pathway of those presenting with DSH to MMCRI highlighting that only a few receive psychosocial assessment. A working group of psychiatrists, psychologists, social workers, casualty medical officers, statisticians and hospital managers was formed to arrive at a consensus on the minimum dataset that could be gathered from DSH survivors for the purpose of setting up a register. Literature on establishing self-harm registers was reviewed along with international guidelines in relation to self-harm assessment in the general hospital.22, 23 Opinion was sought from senior psychiatrists and public health personnel from the private and public sector in Mysore and from the United Kingdom (UK). The team was visited, supported and advised by the Centre for Mental Health and Society, Bangor, UK.
The items listed in Table 1 were considered as ‘minimal yet essential’ for informing clinical practice, service development and patient engagement in future research. The study was not externally funded and, due to time and resource implications, it was agreed that outcomes of mental health assessments would not be recorded in the register. The method of DSH was coded according to the International Classification of Diseases 10th Revision (ICD-10) criteria24 and socio-economic indicators were derived from a modified Kuppuswamy’s scale25 that is validated for the south Indian urban population.
Table 1. Contents of the deliberate self-harm (DSH) register.
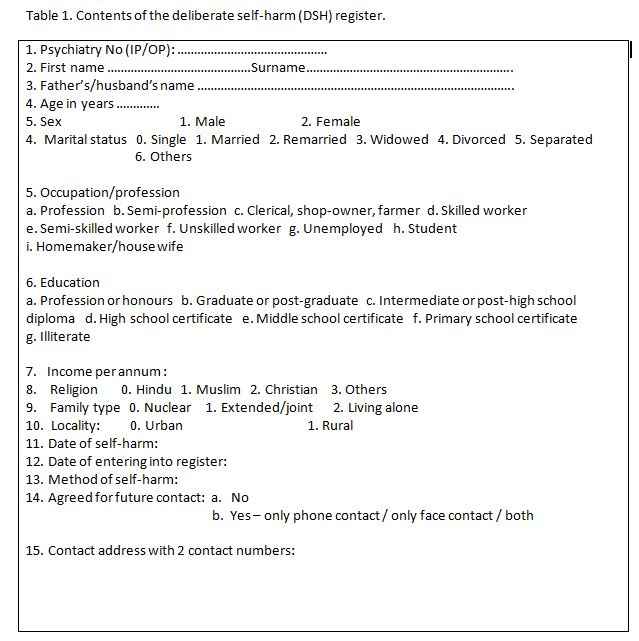
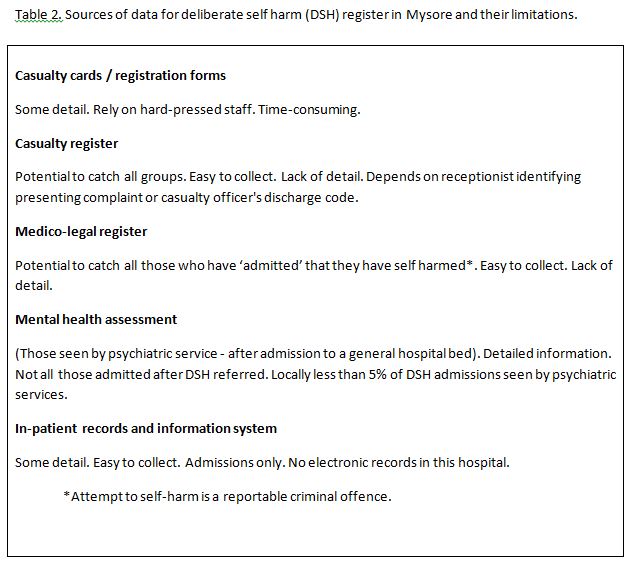
An electronic DSH register was set up in February 2013 and is currently held in the Department of Psychiatry, MMCRI, and Mysore. Two pre-registration House Officers (junior resident equivalent) visited the casualty department daily and identified those cases registered as self-harm from both the standard patient register and medico-legal case registers. If the individual was discharged from casualty (condition necessitated no further treatment, no intensive care bed available, or patient chose admission in private sector after first aid) the available information is captured from the registers and medical records. If they admitted to the general hospital they were traced and personally contacted. Information (as in Table 1) was collected from DSH survivors and from medical records. The data was verified by a Consultant Psychiatrist before being entered in the register. DSH survivors are asked to provide two contact details (postal address and phone number) for future tracing if they consent to further contact either in person or by phone. Table 2 is a list of the sources of data for the DSH register in Mysore and their limitations.
Table 2. Sources of data for deliberate self harm (DSH) register in Mysore and their limitations.
Feasibility
A DSH register should be representative, complete and accurate. The register should be acceptable to the entrants and only take a minimal time for data collection and registration. For the purpose of this study the following were identified as indicators of feasibility:
· Time between identifying that the patient should be included in the register and completion of data entry in the register. This was recorded for 80 randomly chosen inpatient DSH survivors.
· The proportion of patients presenting with alleged DSH who were correctly identified and, if admitted to the general hospital, traced for the purpose of inclusion to the register (representativeness).
· Proportion of those included in the register for whom a full data set could be captured (completeness).
· Proportion of the DSH survivors who were willing to be included in the register and provided contact details for future follow-up (acceptability).
· Over a period of a week, every month during study period February 2013 to July 2013, a Consultant Psychiatrist independently collected data from casualty registers and checked against the total number registered on the DSH register for the corresponding month (accuracy).
RESULTS
Between February 2013 and July 2013, a total of 19,563 patients attended the casualty department. Of these, 1072 attended in relation to self-harm. 1041 of them were hospitalised for further intervention. All of those who were hospitalised and survived (n=817) were traced and contacted. None objected to their details being entered on the register. However, only 253 of the 817 (30.9%) agreed to be contacted for future follow-up. Of the 817, only 109 (13%) had been formally referred to the psychiatry department for an assessment prior to contact with the research team. None of the 817 had any involvement with Social Services.
Out of the 1023 on the register, complete data was available and/or obtained for 740 (72.3%) individuals and data was incomplete for 283 (27.7%) patients. Either by reviewing the medical records or interviewing the patient, it was confirmed in all 1023 cases that there had been an act of self-harm necessitating medical intervention. The time between identifying that the patient should be included in the register and completion of data entry in the register varied between 30 minutes and 2 hours. When the data collected was cross-verified (n=315) by a Consultant Psychiatrist (author RR), entries of 310 individuals were accurate, with a minor discrepancy in less than 3 items for another 5 individuals.
Various terminologies were used to report a case of DSH in the case records (for example, suicide attempt, failed suicide, self-harm, poisoning, deliberate harm).
DISCUSSION
This is the first description of a method of successfully setting up and maintaining a DSH register in an Indian setting. It was a labour-intensive exercise due of lack of electronic patient data management, administrative support and the absence of an agreed care pathway for DSH in the hospital. Despite these obstructions, we have illustrated that it is feasible to set up a DSH register in a busy tertiary care hospital in India. Results of our study indicate that the register details are accurate and representative of those who seek help from the specialist centre. However, it cannot capture those patients whose DSH was managed successfully within primary health centres, those individuals who failed to seek help and those who died before admission.
Clinical Implications
The experience of establishing a DSH register has lead to changes in local clinical practice. DSH is associated with increased morbidity and increased utilisation of health services.26 DSH survivors who were contacted (n=817) by the psychiatry residents were offered psychosocial assessments. Under normal circumstances, 708 (87%) of this group would not have received any psychosocial assessment. The process of setting up the register has helped to identify DSH cases so that an intervention can be offered before discharge from the general hospital. The register has also played a major role in the identification of people who harmed themselves but were discharged without admission to a ward. This group can also be helped. We have now developed an education and service information leaflet which includes emergency contact details (similar to a crisis card in the UK), which is given to DSH patients on discharge. These are known to decrease the repetition of DSH in the developed world.27 Deaths from suicide are largely preventable if knowledge and understanding of this maladaptive behaviour is used to ensure timely intervention.8
By auditing DSH data in a systematic way, clinical decision-making will be based on pooled experience, not just on each clinician’s recall. Comprehensive registers of DSH provide clinicians with the opportunity to review cases of suicide where they have had clinical involvement, using techniques such as psychological autopsy, improving clinical skills and judgements. Overall there is a need for an attitude of vigilance about suicide risk, and of enthusiasm about pursuing initiatives for suicide prevention based on evidence. Better understanding of self-harm will assist in devising means of reaching out to those at risk of dying without having had contact with health care services.
Reporting of DSH in case records was inconsistent. There is a need for uniform recording, medical coding and reporting of DSH. In the DSH register, the method of self-harm is recorded using an international recognised coding system (e.g. ICD-10).
If we continue to offer psychiatric assessment to all cases of DSH, the much higher rate of ascertainment arising from the DSH register will place further strain on an already stretched psychiatric service. Further investment in services specifically targeting self-harm in India is urgently needed.
Service Implications
Use of the register
The register creates an opportunity for a standing DSH audit, allowing for identification of trends over time and comparisons with other services that establish DSH registers using similar methods. Systematic collection of demographic and clinical data will allow calculation of admission rates, repetition rates and other indices of importance in service development. Collaboration with non-governmental organisations in the region who work with those who self-harm will allow development and evaluation of specific culturally appropriate interventions.
Where the register should be held?
In the developed world DSH registers are normally held on electronic systems in the Accident and Emergency department or liaison psychiatric services. In India, it is a mandatory obligation to hold a medico-legal register (which includes DSH) in casualty. Maintaining an additional DSH register risks unnecessary duplication, but modification of a medico-legal register creates an ethical problem and risks under-reporting. There are few liaison psychiatry services in India. On balance, we suggest that our practice of holding the DSH register within the department of adult psychiatry is the optimal arrangement in the Indian setting.
Confidentiality
Confidentiality must be respected. In the UK, when establishing a DSH register, it is necessary to discuss issues of confidentiality and legality with the local Data Protection Officer, and to register under the Data Protection Act. Use of the data for research purposes requires approval from local Research Ethics Committees. In India, there is little regulation of this sort. In order to establish our register it was only necessary to obtain consultant approval and consent through the local medical committee. We suggest that good practice would demand that standards of confidentiality and oversight should, as far as possible, match Western standards.
Manpower and resources
Setting up this register in Mysore required input by a Consultant Psychiatrist, for 2 sessions per week for 6 months, to negotiate with casualty medical officers, consultant physicians and reception staff. The resident from the psychiatry department spent at least 2 hours a day collating and updating the register. The absence of a patient electronic data system and lack of administrative support has placed additional strain on residents and has prolonged the time to identify a case of DSH from the casualty records and trace them on the medical wards. We believe that once the register is established, these tasks could be managed by a trained Social Worker spending 1 session per day collecting the data and 1 session per week editing the register. The work load might vary in other hospitals, depending on the number of daily hospital attendances for DSH.
Integration with other data sources
Linking this register with post mortem records, local civil registration of deaths and police records is desirable but this needs co-ordinated effort from several civil bodies and public health organisations. In the absence of any legislation or national record linkage systems, there are few motivators to drive this change or the allocation of resources. However, a unique person identification number system is presently being rolled out across India. The development of cross-agency electronic databases will facilitate easier record linkage in the future, which creates the opportunity for collection of reliable and representative data at a regional level.
None of those who were contacted during the study period had any formal input from Social Services. Though the models and mode of delivery by Social Services in India is radically different to those in Europe, DSH survivors form a stigmatised vulnerable group who are frequently in need of social assessment and support.
Future investment and development
There are good humanitarian reasons to seek the de-criminalisation of acts of self-harm in India, and there is presently strong lobbying to bring this about. It is reasonable to suppose that this might lead to readier help-seeking and better reporting of self-harm and suspected suicide. However, there are other measures that would be necessary to reduce rates of DSH and completed suicide. Regulating the supply of organophosphate insecticides, so that they are only available in dilutions that make fatal overdose more difficult, would be one such measure. There is also a need to develop liaison psychiatric services, offering psychosocial assessments to a higher proportion of those who present with features indicative of probable self-harm. Other necessary developments include investment in patient electronic records and systematic strategies for destigmatisation of DSH.
The register has provided us with a cohort of individuals who are willing to be contacted for future studies. The register has continued beyond the study period. We presently have 3720 individuals on the register. The unit has established formal links with research centres in the UK. We intend to carry out longitudinal studies to examine the patterns of DSH, rates of repetition, compliance with follow-up and suicide rates. This will help to identify the culture-specific access, adherence and prognostic factors, and will influence the development and validation of brief psychosocial interventions in a social, economic and cultural context that is radically different to the West.
CONCLUSIONS
We have illustrated that it is feasible to set up a DSH register in a busy tertiary care hospital in India where rates of self-harm are high. Results of our study indicate that the register details are accurate and representative of those who seek help from the specialist centre.
Very few were referred for psychosocial assessment following an act of self-harm and none of them had any formal input from Social Services. Though the models and mode of delivery by Social Services in India is radically different to those in Europe, DSH survivors form a stigmatised vulnerable group who are frequently in need of social assessment and support.
|
Acknowledgements We thank Prof Raveesh, Head of the Department of Psychiatry MMCRI, Mysore, India and Prof Geeta Avadani Dean MMCRI Mysore for providing access to the hospital records, casualty and wards. Competing Interests None declared Author Details RAJAGOPAL RAJENDRA, Associate Professor, Department of Psychiatry, Mysore Medical College and Research Institute, Mysore, India. MURALI KRISHNA, Early Career Research Fellow, Wellcome Department of Biotechnology (DBT) Alliance and Consultant Psychiatrist at CSI Holdsworth Memorial Hospital, Mysore, India. SUMANTH M MAJGI, Assistant Professor, Department of Community Medicine , Mysore Medical College and Research Institute, Mysore, India. NARENDRA HEGGERE, Assistant Professor in Psychiatry, Department of Psychiatry, Mysore Medical College and Research Institute, Mysore, India. CATHERINE A. ROBINSON, Professor of Social Policy Research, Centre for Mental Health and Society, School of Social Sciences, Bangor University, United Kingdom. ROB POOLE, Professor of Social Psychiatry, Centre for Mental Health and Society, School of Social Sciences, Bangor University, United Kingdom. CORRESPONDENCE: DR MURALI KRISHNA, Early Career Research Fellow, Wellcome DBT Alliance and Consultant Psychiatrist at CSI Holdsworth Memorial Hospital, PO Bo 28 Mandi – Mohalla, Mysore, India PIN 570021 Email: muralidoc@gmail.com |
References
1. Aaron R, Joseph A, Abraham S, Muliyil J, George K, Prasad J, Minz S. Suicides in young people in rural southern India. Lancet 2004; 363:1117-1118.
2. Bose A, Konradsen F, John J, Suganthy P, Muliyil J, Abraham S. Mortality rate and years of life lost from unintentional injury and suicide in South India. Trop Med Int Health 2006; 11: 1553-1556.
3. Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 2007; 7:357.
4. World Health Organization Suicide prevention (SUPRE). Retrieved March 18, 2011 from http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
5. Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, Jha P. Million Death Study Collaborators. Suicide mortality in India: a nationally representative survey. Lancet 2012; 379(9834):2343-2351.
6. National Crime Records Bureau (NCRB) New Delhi: National Crime Records Bureau (NCRB); 2010. Accidental deaths and suicide. www.ncrb.nic.in.
7. Accidental deaths and suicides in India 2005. (National Crime Records Bureau [NCRB], Ministry of Home Affairs, New Delhi, 2006).
8. World Health Organization. Emerging from darkness. Mental health and substance abuse facts and figures suicide prevention: South East Asia, 2007.
9. Hawton K, van Heeringen K. Suicide. Lancet 2009; 373(9672): 1372-1381.
10. World Health Organization. The World Health Report 2001. Mental health: new understanding, New Hope, Geneva, 2001.
11. Radhakrishnan R, and Andrade C. Suicide: An Indian perspective. Indian J Psychiatry 2012; 54(4): 304-319.
12. Joseph A, Abraham S, Muliyil JP, George K, Prasad J, Minz S, Jacob KS. Evaluation of suicide rates in rural India using verbal autopsies, 1994-9. BMJ 2003; 326:1121-1122.
13. Bose A, Konradsen F, John J, Suganthy P, Muliyil J, Abraham S. Mortality rate and years of life lost from unintentional injury and suicide in South India. Trop Med Int Health, 2006; 11:1553-1556.
14. Prasad J, Abraham VJ, Minz S, Abraham S, Joseph A, Muliyil J P, Jacob KS (2000). Rates and factors associated with suicide in Kaniyambadi Block, Tamil Nadu, South India, 2000–2002. Int J Soc Psychiatry 2000; 52:65-71.
15. Gajalakshmi V, Peto R. Suicide rates in rural Tamil Nadu, South India: Verbal autopsy of 39 000 deaths in 1997–98. Int J Epidemiol, 2007; 36(1): 203-207.
16. Bhat M. Vol. 7. Minneapolis, MI, United States: Centre for Population Analysis and Policy, Humphrey Institute of Public Affairs, University of Minnesota; Mortality from accidents and violence in India and China, Research Report 91-06-1, 1991.
17. Ruzicka LT. Suicide in countries and areas of the ESCAP region. Asia Pac Popul J, 1998; 13(4):55-74.
18. Yadwad BS, Gouda Hareesh S. Is attempted suicide an offence? Journal of Indian Academy of Forensic Medicine, 2005; 7(2):108-111.
19. Accidental Deaths and Suicides in India 2008. National Crime Records Bureau [NCRB], New Delhi: Ministry of Home Affairs, Government of India, 2010.
20. Eddleston M, Buckley N A, Gunnell D, Dawson AH, Konradsen F. Identification of strategies to prevent death after pesticide self-poisoning using a Haddon matrix. Inj Prev, 2006; 12:333-337.
21 World Health Organization. Suicide rates per 100,000 by country, year and sex. 2011 Retrieved from http://www.who.int/mental_health/prevention/suicide_rates/en/index.html
22. National Institute for Health and Care Excellence. Self-harm: the short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. NICE clinical guideline 16. 2004.
23. National Institute for Health and Care Excellence. Self-harm: longer-term management. NICE clinical guideline CG133.2011.
24. World Health Organisation. ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. Geneva. World Health Organisation.1992
25. Sharma, R. Kuppuswamy's socioeconomic status scale - revision for 2011 and formula for real-time updating. Indian J Pediatr 2012; 79(7):961-962.
26. Evans J, Johnson C, Stanton R. How to establish case registers: II. Non-fatal deliberate self harm. Psychiatric Bulletin 1996; 20:403-405.
27. Evans MO, Morgan HG, Hayward A. Crisis telephone consultation for deliberate self harm patients: effects on repetition. British Journal of Psychiatry 1999;175: 23-27.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




