Frequency and severity of depression among mothers of children with cancer: Results from a teaching hospital in Karachi, Pakistan
Mariam Ghufran, Marie Andrades and Kashmira Nanji
Cite this article as: BJMP 2014;7(1):a701
|
|
Abstract Background: Diagnosis of cancer in one’s child causes not only social but also psychological devastation for the whole family especially mothers. Depressed mothers are less able to help their sick child cope with intensive treatments. This study was doneto identify frequency and severity levels of depression in mothers of children with cancer. Abbreviations: AKUH (Aga Khan University Hospital), HAM-D (Hamilton- Depression Scale), WHO (World Health Organization), CDC (Centers for Disease Control and Prevention), ALL (Acute Lymphoblastic Leukemia), SPSS (Statistical Package For Social Sciences), US (United States), GNP (Gross National Product), NCI (National Cancer Institute, SD (Standard Deviation), SEER (Surveillance Epidemiology and End Results), CI (Confidence Interval), OR (Odds Ratio) |
Introduction
Currently, depression is the leading cause of disability in the world and is predicted to become the second largest killer after heart disease by the year 20201. Eighty percent of individuals with depression report functional impairment while 27% report serious difficulties at work and home life2. According to a study conducted in 2011, India has the highest rate of depression (36%) in low income countries with women being affected twice more than men3. Cancer in children occurs randomly and spares no ethnic group, socio-economic class, or geographical region. An estimated 11,630 new cases are expected to occur among children aged 0-14 years in 2012 in the US, out of which 1,310 will die by end of 2013 due to it4. Based on Karachi Cancer Registry it is estimated that about 7500 children get cancer every year in Pakistan5. The mortality rates for childhood cancers have declined by 68% over the past four decades, from 6.5 per 100,000 in 1969 to 2.1 in 20094. However, the diagnosis of cancer in one’s child marks the beginning of social and psychological devastation for the whole family especially the mother. The length and intensity of treatment can be as distressing as the disease itself, negatively affecting their functionality as parents and in turn the child’s ability to handle the treatment6. As a primary care provider mother’s responsibility increases substantially starting a vicious cycle of anxiety and socio-economic uncertainty leading her to depression much more than the father7. The available data supports that mothers of children with cancer represent a group prone to high levels of emotional distress, and that the period following their child’s diagnosis and the initiation of treatment may be predominantly stressful and disturbing leading them to depression8. Such mothers have difficulty in taking care of themselves, their household and especially their sick children. Many parents continue to suffer from clinical levels of distress, even after five years off treatment of their child7. Many studies have shown that chronic depression and distress may lead to decrease in immune functioning and an increased risk of infectious disease in healthy individuals 9-11. Mothers are generally with the child mainly and hence are most affected from their child’s disease. In this study, we intended to estimate the frequency and severity of depression in mothers having children with cancer.
There is limited evidence from Pakistan regarding depression in mothers of children with cancer. The previous studies conducted had certain limitations such as small sample size, assessment of depression in both parents and that too of children with leukaemia only. This study intends to determine the frequency and severity of depression among mothers of children with cancer.
Methods
A cross sectional survey was conducted in the paediatric oncology clinics at The Aga Khan University Hospital, a teaching hospital in Karachi over a period of six months (September 2011- March 2012). Mothers of children with cancer were enrolled in the study, consecutively according to the inclusion and exclusion criteria. Mothers having children less than 15 years of age with any type of cancer, diagnosed by oncologist (2 months after diagnosis to rule out bias for normal grief period)12, mothers bringing their sick child for the first time to the teaching hospital or as follow up or for day care oncology procedures were included in the study. Mothers who had existing psychiatric illness (and or already diagnosed as having depression by a doctor) and/or taking medications for it, any recent deaths in family (within six months of interview) or having other co-morbidities (malignancy, myocardial infarction in previous year, neuromuscular disease limiting ambulation or blindness) were excluded.
A pre-coded validated and structured Urdu13, 14 and English15, 16 version of the questionnaire was used for data collection the questionnaire took about 20 minutes to complete and consisted of two sections. Section A, included mother’s and child’s demographic details and treatment status. Section B, consisted of Hamilton Depression Rating Scale (HAM-D 17) a validated scale (sensitivity 78.1% and specificity 74.6%) for assessing frequency and severity of depression in both hospitalised patients and the general population15. Scores of < 7 indicate no depression and scores > 7 are labelled as depressed. Mothers who were found to be depressed were further classified into mild (scores 8-13), moderate (scores 14-18), severe (scores 19-22) and very severe depression (scores > 23)16. Mothers with mild to moderate depression were referred to the family physicians; those with severe, very severe, or suicidal tendencies were urgently referred to a psychiatrist.
Institutional Ethical Committee of the Aga Khan University Hospital approved the study. Confidentiality of participants was maintained and informed written consent was obtained.
Sample sizecalculated by WHO software. The prevalence of maternal depression ranges from 56.5% to 61.5% 17, 18 as evident from different international studies. With 95%, confidence interval and bound on error of 10% the sample size came out to be 95. After an addition of 5% for non-responders, the total required sample size was 100 study participants. Data was double entered and analyzed in SPSS version19. The outcome variable was dichotomized as no depression and depression (cut off score7). Analysis was performed by calculating frequencies of categorical variables (maternal age, education, current marital status, employment, co- morbidities, diagnosed depression and treatment in mother, number of children, gender of sick child, cancer type, time since diagnosis of cancer in child, treatment given so far and current treatment status of child and family income). Means and Standard Deviation was reported for current age of the child.
Results
One hundred and sixty mothers were approached out of which 100 mothers consented to participate in the study yielding a response rate of 62.5% (100/160). With regards to the mothers the most common age group was the 30-39 year old category (43%). Fifty-five percent of mothers had a high level of education (those who had completed class 11-12 or engaged in professional education). Nearly all the mothers (98%) were married and were homemakers (95%). Only 5% of mothers were working outside the home. More than half of the participants (57%) had one to three children while 43% had more than three. Monthly financial income for 65% of the participants were more than fifty thousand Pakistani rupees (Table 1).
Table 1: Demographic Characteristics of Mothers (N=100)
| Variables | N | % |
| Age of mother | ||
| 20-29 years | 39 | 39.00% |
| 30-39 years | 43 | 43.00% |
| 40 years and above | 18 | 18.00% |
| Education Level of mothers* | ||
| No education | 13 | 13.00% |
| Primary/secondary/intermediate | 32 | 32.00% |
| Higher | 55 | 55.00% |
| Marital status of mothers | ||
| Currently Married | 98 | 98.00% |
| Divorced | 1 | 1.00% |
| Widow | 1 | 1.00% |
| Maternal Employment Status | ||
| Housewife | 95 | 95.00% |
| Working | 5 | 5.00% |
| Number of children | ||
| 1-3 | 57 | 57.00% |
| More than 3 | 43 | 43.00% |
| Family Income | ||
| < 20,000 | 4 | 4.00% |
| 20,000-50,000 | 31 | 31.00% |
| >50,000 | 65 | 65.00% |
* (Not Educated: Those who do not have primary education, Primary 1-5 years of schooling, Secondary: 6 to 10 years of schooling, Intermediate: Who have studied class 11 and 12, Higher: Who have completed or engaged in professional education)
The demographic characteristics of child are detailed in Table2. Seventy-five percent of sick children were male while 25% were females (n=100). Half the children were diagnosed with cancer between the age of three to nine. Fifty percent of children (n=50), had their diagnosis of cancer in the last one to five years. More than half of children (57%) were on treatment during study phase. Different types of cancers occurring in children are shown in Figure1.
Table 2: Demographics and social characteristics of sick child (N=100)
| Variables | N | % |
| Current age of child * | 6.90(±3.40)* | |
| Gender of Sick Child | ||
| Male | 75 | 75.0% |
| Female | 25 | 25.00% |
| Age of child at cancer diagnosis | ||
| 10months-3 years | 40 | 40.0% |
| 3 -9 years | 50 | 50.00% |
| More than 9 years | 10 | 10.00% |
| Time since diagnosis of child’s cancer | ||
| < 1 year | 15 | 15.0% |
| 1-5 years | 50 | 50.00% |
| >5 years | 35 | 35.00% |
| Current treatment status of child | ||
| On treatment | 57 | 57.0% |
| Off treatment | 43 | 43.00% |
*Mean (SD) (t-test values)
Figure 1: Frequency of various types of cancer in children (N=100)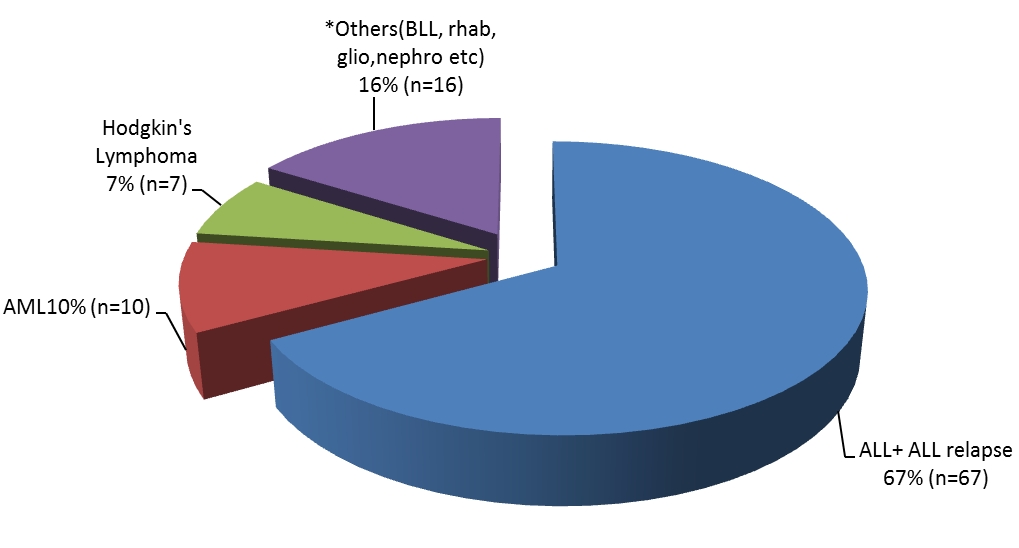
*Others (BLL, Rhabdomyosarcoma, Glioblastoma, Nephroblastoma)
Seventy eight percent of the mothers were depressed. Sixty-nine percent (n= 54) had mild depression, nearly 25% (n=19) had moderate, while 5% (n= 4) had severe and 1% (n=1) had very severe depression.(Table 3)
Table 3: Frequency and levels of severity of Depression in mothers
| Variables | N | % |
| Frequency of Depression (n=100) | ||
| Depression present | 78 | 78% |
| Depression absent | 22 | 22% |
| Severity of Depression (n=78) | ||
| Mild | 54 | 69% |
| Moderate | 19 | 25% |
| Severe | 4 | 5% |
| Very severe | 1 | 1% |
Discussion
Depressed patients are frequently encountered in nearly all specialty clinics. However, depression in caregivers accompanying patients is usually overlooked and hence missed, as doctors are mostly focused on the patient’s evaluation, condition, and treatment. When the patient is a child and the diagnosis is cancer, this difficult circumstance has a sudden and long term impact on both the child and the family. Many parents of a child with cancer will have very strong feelings of guilt. As such, parents of cancer survivors may be at risk for impaired physical and mental health. An increasing body of literature supports the conclusion that various levels of parental distress are ongoing, long after treatment is completed 19, 20.
The prevalence of depression in mothers in this study was as high as 78%. Mild depression was seen in 69% of mothers, moderate in 25%, severe in 5% while 1% had very severe depression. This high prevalence of depression in such mothers has not been reported from Pakistan before. The soaring levels of depression however have been consistent with the study conducted in Turkey in 2009 in mothers of children with leukaemia21 where 88% (n=65) mothers were depressed. Mild depression was reported in 22.7 % (n=18) and major depression in 61.5% (n=40). Similar results were reported from a study conducted on both parents of children with leukaemia in 2002 in Pakistan where 65% (n=60) of mothers were found to be depressed 17. Nevertheless, severity of depression in this study was not noted. A Sri Lankan study in 2008, showed moderate to severe depression to be 22.9% and 21.9% in mothers having children with mental and physical disorders respectively22. Another study conducted in Florida in 2008 suggests that an increased symptom of depression in mothers is related to significantly lower ratings in quality of life for their children18.
The existing data supports the argument that mothers of children with cancer represent a group prone to high levels of emotional distress. The time following their child’sdiagnosis and the commencement of treatment may be particularly stressful and traumatic 23 with an incidence as high as 40% 24-26. There could be multi-factorial reasons for this alarmingly high rate of depression seen in Pakistani mothers. One of the causes could be the political instability that Pakistan has been facing for past few years leading to economic volatility. The study conducted in 2002 in Karachi saw 65% of maternal depression17 which has now risen to 78% in this study. Due to political unrest, everyday strikes, bombasts, these mothers may also have difficulty in reaching hospital on scheduled visits leading to postponement of treatment. Other reason could be economic inflation. The cost of daily living has soared while allocated medical budget was 0.27% of its gross domestic product (GDP) on health in 2011-12, which is insufficient to cater the needs of the population (Economic Survey of Pakistan of 2011-2012).
Lately, there has been a recent trend towards nuclear families in Pakistan rather than living in extended families as before27. This in turn may lead to mother being the soul person in looking after the sick and her healthy children as well as managing house chores and doctor’s appointments leading to more frustration. This study also showed that 57% mothers had three children while 43% had more than three children. This could also be one of the factors for high rate of depression as looking after multiple children is demanding and may lead to decreased coping skills of mothers.
Other possible reason for this high rate of depression could be that mostly educated mothers were visiting the hospital that have access to internet and can search up all details, good or bad, on their child’s disease. This may start a vicious circle of worry for mothers. Other possible reasons for this growing depression could be gender of child (as in this society male child is thought to be the support and bread earner of the family), child’s current treatment status and time since diagnosis of cancer in child.
Strengths and Limitations
To the best of authors’ knowledge, this study has touched upon a topic that was not yet been attended to, in local context. Moreover, in this study adjustment phase of two months, for acute stress and posttraumatic stress disorder was given for diagnosis of depression in mothers. It was done to rule out bias in study. HAM-D also focuses on symptoms in the past 1 week, to minimize the recall bias. The findings in this study offer evidence and importance of the need for developing psychological support for families especially mothers who are caring for a child with cancer, in Pakistan.
This study has several limitations. The study was conducted in a tertiary care private hospital, which mostly caters a specific segment of population. Hence, the results may not be a true representation of the population. All data in this study was self-reported by the participants. Thus, it is anticipated that there may be some bias in their responses and recall. Lastly, since this was a cross-sectional study so temporality is difficult to establish.
Conclusion
In conclusion more than three-fourth of our study participants were depressed.
The outcome is expected to identify depressed mothers so that effective strategies can be developed to enhance their coping skills and medically treat them when required. This in the long term is expected to increase quality of life for both their sick and healthy children as well as mothers themselves.
Future Research and Policy Recommendations
Future studies are recommended in order to confirm our findings. Such studies need to be conducted on a larger scale, at national level, in various hospitals and settings to counteract limitations of our study with appropriate means of measuring depression in mothers. Factors, not explored in this study such as personality styles and coping skills of mothers can be explored as these may be significant aspects leading to depression. Further co-morbidities, such as anxiety and post traumatic stress disorder symptoms related to child’s cancer should also be investigated.
Other associated factors, such as the political and economic situation, which perhaps may also be a leading cause of depression in our part of the world, should also be assessed. Simultaneously, measures should be taken to root such factors out at national levels.
The results of current study show the need of incorporating mothers into a treatment process designed for psychological interventions, not only after the diagnosis of cancer in their child but also during their child’s treatment. Psychosocial services should be recognised as an important constituent of comprehensive cancer care for families of children with cancer.
It is highly advocated that the healthcare professionals who work with the families of children with cancer should evaluate the children and their families concerning the psychological and social aspects of their lives. Arrangements for family counselling for those needing help should be made. Mothers should also be referred to family physicians and social support if available. The mother’s crucial position in the family and the proximal and distal effects of her adaptation to the crisis of cancer in the family should lead to the design of interventions intended at decreasing her distress and at promoting her adaptive coping skills as improving mothers’ problem-solving skills has been associated with reductions depression and anxiety28. Thus, all hospitals, dealing with paediatric cancer cases should have a family counselling and support system.
|
Acknowledgements The authors thank Peadiatric Oncologists Dr. Zehra Fadoo and Dr. Naureen Mushtaq for easy access to their patients Competing Interests None declared Author Details MARIAM GHUFRAN, FCPS(FAMILY MEDICINE), MRCGP (INT),Department of Family Medicine, Aga Khan University Hospital, Stadium Road, P.O. Box 3500,Karachi-74800, Pakistan. MARIE ANDRADES, ASSOCIATE PROFESSOR & PROGRAM DIRECTOR FAMILY MEDICINE, Aga Khan University Hospital, Karachi, Pakistan. KASHMIRA NANJI, EPIDEMIOLOGIST,Department of Family Medicine, Aga Khan University Hospital, Karachi, Pakistan. CORRESPONDENCE: Dr. MARIAM GHUFRAN, Department of Family Medicine, Aga Khan University Hospital, Stadium Road, P.O. Box 3500,Karachi-74800, Pakistan. Email: mariamghufran@hotmail.com |
References
- WHO. Mental health. Mental health disorders [URL: http://www.who.int/mental_health/management/depression/definition/en/. Accessed Jul 22, 2012.
- CDC. NCHS Data Brief:Death in the United States, 2010. URL: http://www.cdc.gov/nchs/data/databriefs/db99.pdf. Accessed Jun 13, 2012.
- Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC medicine. 2011 Jul;9(1):90.
- American Cancer Facts and Figures. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf. Accessed Feb 12, 2013.
- Childhood Cancers. Children Cancer Foundation Karachi. URL: http://ccfpakistan.org/2011/05/23/childhood-cancer/. Accessed Jan 15, 2012.
- Steele RG, Dreyer ML, Phipps S. Patterns of maternal distress among children with cancer and their association with child emotional and somatic distress. J Pediatr Psychol. Oct 2004;29(7):507-517.
- Wijnberg-Williams BJ, Kamps WA, Klip EC, Hoekstra-Weebers JE. Psychological distress and the impact of social support on fathers and mothers of pediatric cancer patients: long-term prospective results. J Pediatr Psychol. Sep 2006;31(8):785-792.
- Dolgin MJ, Phipps S, Fairclough DL, et al. Trajectories of adjustment in mothers of children with newly diagnosed cancer: a natural history investigation. J Pediatr Psychol. Aug 2007;32(7):771-782.
- Cohen S, Doyle WJ, Skoner DP. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosom Med. 1999 Mar-Apr;61(2):175-180.
- Robles TF, Glaser R, Kiecolt-Glaser JK. Out of Balance A New Look at Chronic Stress, Depression, and Immunity. Current Directions in Psychological Science. 2005;14(2):111-115.
- Kiecolt-Glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neurosci Biobehav Rev. Sep 2010;35(1):33-38.
- Kendler KS, Myers J, Zisook S. Does bereavement-related major depression differ from major depression associated with other stressful life events? The American journal of psychiatry. 2008 Aug;165(11):1449.
- Raza-Ur-Rahman MAA, Siddiqui AA, Akunzada WA, Hayder Z, Luhano ML. Correlation of Urdu Version of Hospital Anxiety Depression Scale and Hamilton Depression Rating Scale in Quantifying Depression among Post-Myocardial Infarction Patients. JLUMHS. 2009;8(02):131.
- Siddiqui A, Syed EU. Comparison of Vitamin B12 Supplementation to Selective Serotonin Reuptake Inhibitor (SSRI) Versus SSRI Antidepressant Treatment Alone. Karachi: Aga Khan University; 2009.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. Feb 1960;23:56-62.
- Jha SK. Depression scales.Current Medicine Group. Dec 20; URL: http://www.cnsforum.com/clinicalresources/ratingscales/ratingpsychiatry/depression. Accessed Dec 18, 2011.
- Iqbal A, Siddiqui KS. Depression among parents of children with acute lymphoblastic leukemia. J Ayub Med Coll Abbottabad. Apr-Jun 2002;14(2):6-9.
- Roddenberry A, Renk K. Quality of Life in Pediatric Cancer Patients: The Relationships Among Parents’ Characteristics, Children’s Characteristics, and Informant Concordance J Child Fam Studies. 2008 Mar;17(3):402-426.
- Hutchinson KC, Willard VW, Hardy KK, Bonner MJ. Adjustment of caregivers of pediatric patients with brain tumors: a cross-sectional analysis. Psycho-oncology. May 2009;18(5):515-523.
- Hutchinson KC. Parental adjustment: An examination of caregivers of pediatric cancer survivors. online Thesis, DUKE UNIVERSITY; 2010.
- Erkan S, Kaplan Y. A study on the depression levels of mothers of leukemic children. Pak J Soc Sci. 2009 Sept;6(1):42-47.
- Perera H, Mudalige CDK, Karunaweera H, et al. Prevalence of depression in mothers of children suffering from psychiatric and physical disorders. J Sri Lanka Child Health. 2008 Jan;37(2):42-47.
- Sawyer M, Antoniou G, Toogood I, Rice M, Baghurst P. Childhood cancer: a 4-year prospective study of the psychological adjustment of children and parents. J Pediatr Hematol Oncol. May-Jun 2000;22(3):214-220.
- Brown RT, Madan-Swain A, Lambert R. Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. J Trauma Stress. Aug 2003;16(4):309-318.
- Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. Apr-May 2004;29(3):211-219.
- Kazak AE, Boeving CA, Alderfer MA, Hwang WT, Reilly A. Posttraumatic stress symptoms during treatment in parents of children with cancer. J Clin Oncol. Oct 20 2005;23(30):7405-7410.
- Alam A. Factors and Consequences of Nuclearization of Family at Hayatabad Phase-II, Peshawar. Sarhad J. Agric. 2008.
- Sahler OJ, Varni JW, Fairclough DL, et al. Problem-solving skills training for mothers of children with newly diagnosed cancer: a randomized trial. J Dev Behav Pediatr. Apr 2002;23(2):77-86.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




