Have Crisis & Home Treatment Teams become a Second Opinion or Diagnostic Service?
Pearl Ogaku, Annabel McDonald, Sheeba Hakeem & M Aamer Sarfraz
Cite this article as: BJMP 2018;11(2):a1118
|
|
Abstract Purpose: To investigate the evolving role of Crisis Resolution and Home Treatment Team (CRHTT) within patient care pathway. |
Introduction
There have been continuing initiatives to transform and improve the National Health Service (NHS) in recent years. Mental health services in England have similarly shown evolution with regards to service provision. There has been a shift away from the perceived “medicalisation” of treatment, with traditional long-stay institutions replaced with more targeted and personalised care in the community.1 Furthermore, community services themselves have seen much remodelling over the years including decommissioning and integration, as well as increased involvement in outreach and early intervention teams.2
Mental health services are sometimes perceived as relatively well funded from outside but, as with most healthcare sectors, compared to the population requiring this service, these resources are inadequate to support the growing demand. This has been the case for some time, but it has become more evident with a significant reduction in funding observed since 2010/11.1 In addition, constant governmental pressures to meet key performance targets, as well as unachievable expectations from the public, have further stretched an already resource-depleted mental health service.
The implementation of new National policies3 was supposed to be a shift from large psychiatric hospitals to smaller specialist community centres with a promised reduction in the demand placed on inpatient services. In England, a peak number of 150,000 inpatient psychiatric beds was reported in 1955; this has since rapidly declined to 22,300 in 2012. Between 2010/11 and 2013/14, a further rapid reduction of 7% of all beds available was seen.4
Despite the promise of changes in service delivery within mental health to mitigate the continued reduction in the number of inpatient beds, demand for inpatient beds has not in fact reduced nationally.1 The recommended level of occupancy, for example, is 85% but 119 wards surveyed5 were operating at 91%, with some at 138% level of occupancy. The occupancy levels of over 100% usually occurred when long-stay inpatients were discharged home on short-term leave and their beds got filled during their absence.4 Where numbers of inpatient beds fail to meet the demands, or waiting list for their first assessment or review grows, the inadequacy lends these facilities to issues with regard to providing high quality and safe patient care. Examples of this may include inappropriate use of the Mental Health Act for detention of patients as a means of securing an inpatient bed,5 incomplete assessments of people detained in places of safety due to time or space constraints,6 and an increase in violent incidents on overcrowded inpatient wards.7
What is a Crisis Resolution and Home Treatment Team (CRHTT)?
In the late 1980s and 1990s, community mental health teams provided acute crisis support. This posed a number of issues including that these teams usually operated during normal working hours of 9am-5pm (Monday to Friday) and were not always available to provide support to patients in a crisis, and did not have the desired impact of reducing the number of acute admissions.8 This gap in service provision inspired the experimentation with and subsequent development of intensive home treatment services, some of which showed evidence of reduced hospital admissions, and holistic-working often preferred by families who were happy to have their loved ones receive the required support in the home environment.9 Over the last two decades, with remodelling of services, increased investment, NHS funding rising from £49 billion in 2000 to £122 billion in 2016, and a migration of mental health professionals, CRHTTs were established and are now available in every mental health trust across the United Kingdom (UK).10
CRHTT is a team of mental health professionals including psychiatrists, community psychiatric nurses, social workers and support workers, who provide rapid and intensive support at home during a mental health crisis.11 They are a 24-hour service operating seven days a week, and acting as the “gatekeeper” for acute services accepting referrals from various sources including inpatient, community, liaison and from outside the Trust for providing support to patients experiencing crises. These teams risk-assess patients and determine whether they require inpatient or home treatment. In the latter case, CRHTTs provide intensive home treatment by offering up to 2-3 visits a day as well as 24/7 phone support. These teams are also involved in facilitating early discharges from hospitals; in cases where patients are past the initial acute crisis, but may need further input prior to discharge to community mental health teams for longer term support.8
Definition of diagnosis and second opinion.
A second opinion is defined as “advice from a second expert (such as a doctor/psychiatrist) to make sure advice from the first such expert is correct” whilst diagnosis is defined as “the art or act of identifying a disease from its signs and symptoms”.12 Due to increased pressure on inpatient facilities and remodelling of community services, there has been a huge increase in the number of referrals made to CRHTTs. Between 2011/12 and 2013/14, it has been noted that referrals to CRHTTs increased by 16%.13 Reduction in inpatient beds and high workloads within community services often result in the formulation of arbitrary diagnoses and treatment plans. With increased pressures on other mental health services, the role of CRHTTs has begun to evolve. In addition to the previously discussed functions, CRHTTs appear to be becoming second opinion services by default enabled by the psychiatrists working in these teams.
We organised a project to establish whether a typical CRHTT is fulfilling the criteria of being a diagnostic or second opinion service provider.
Method
We examined 100 consecutively accepted referrals to a CRHTT from 1st December 2016. The patients were divided into three groups: those being discharged/referred from hospital (HR), those referred from the community (CR), and those who were not open to secondary mental health services at the time of referral (NR). The age range and gender of the groups were noted. Thereafter, the NR group was excluded from analysis for the obvious reason that the CRHTT was not providing a second opinion in their case. The HR and CR groups were further reduced by excluding patients who were not seen by a CRHTT psychiatrist. The remaining patients in both groups were scrutinised regarding a change in medication; this was also recorded for the previous and next care occasions. The likelihood of medication change at the next treatment event was analysed to establish whether it was affected by the previous event. The numbers of patients with CRHTT diagnosis change were also recorded for both groups.
Results
Figure 1: Project Flowchart
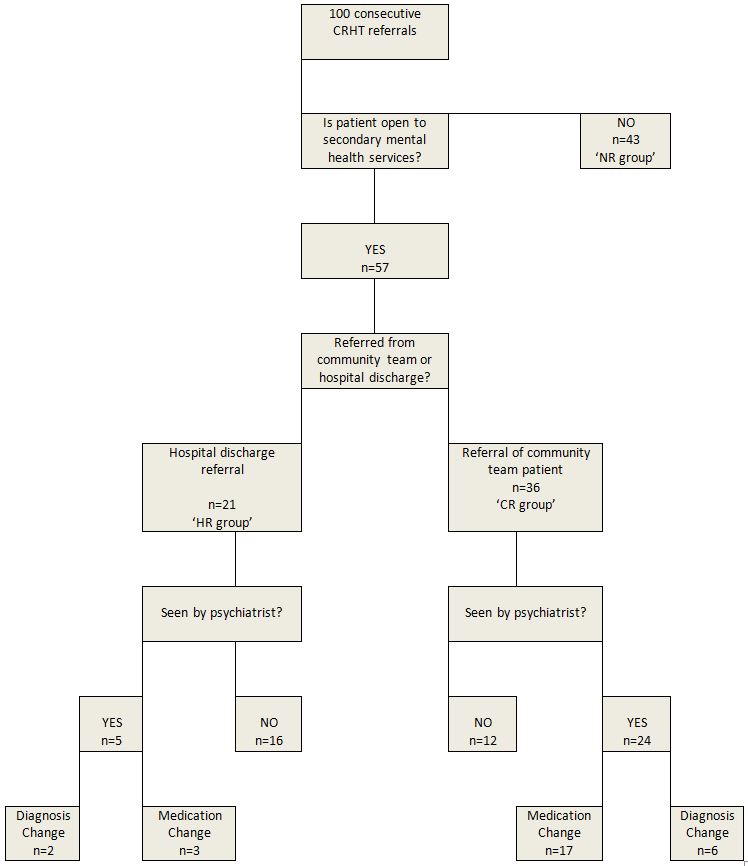
Figure 2: Group Demographics
|
n |
Patient Gender |
Patient Age |
Time with CRHTT |
||||
| Male | Female | Average | Range | 1-7 days | > 7 days | ||
| No prior referral open (NR) | 43 | 20 (47%) | 23 (53%) | 36.0 | 19-60 | 5 (12%) | 38 (88%) |
| Community referral (CR) | 36 | 13 (36%) | 23(64%) | 37.8 | 19-66 | 7 (19%) | 29 (81%) |
| Hospital referral (HR) | 21 | 10 (48%) | 11 (52%) | 39.0 | 19-63 | 6 (29%) | 15 (71%) |
There was little difference in age between the three groups (average ages were: CR=37.8, HR=39.0, NR=36.0). There was a lower proportion of men in the CR group than were present in the HR and NR groups (36% as against 48% and 47%). Whether a psychiatrist saw a patient appeared to be related to both the referral source and the length of CRHTT stay. Most (n=16, 76%) patients in the hospital-referred group (HR) were not seen by a psychiatrist while most (n=24, 67%) of those referred from the community (CR) did receive such an outcome. No community-referred patient was seen by a psychiatrist if they were with the CRHTT for less than a week. These short-stay patients accounted for 7 out of the 12 community-referred patients who were not seen. This suggests that a psychiatric assessment should be scheduled more quickly after community referrals so as to offer patients a more comprehensive service.
Psychiatric assessment led to changed diagnoses for 28% (8/29) of patients. This figure was 40% (2/5) for the HR group and 25% (6/24) for the CR group.
Medications were changed for 69% (20/29) of patients seen by a psychiatrist. In the subgroups; 60% (3/5) of HR psychiatric assessments resulted in a change of medication while 71% (17/24) of CR psychiatric assessments led to medication changes.
The chi-square statistic was used to evaluate whether a recent medication change, during the inpatient stay or at the most recent outpatient appointment, made the CRHTT less likely to adjust medication. This indicated that there was no relationship between the two events. A similar analysis indicated that the likelihood of a medication change at the patient’s next community appointment was increased by seeing a CRHTT psychiatrist but unrelated to whether that assessment had resulted in a change of medication.
Discussion
We have demonstrated in this study that a typical CRHTT is providing a diagnostic and second opinion service. Changes in medication were more than twice as frequent as changes in diagnosis – this is perhaps unsurprising as diagnostic changes would be likely to require a different prescription.
Most community referrals were actively evaluated in terms of both diagnosis and treatment. This is a significant change to the original function of the CRHTT where a psychiatric assessment was not a standard aspect of care when very few of the original CRHTTs included a psychiatrist. This may also reflect the current pressures on community teams, which are frequently short-staffed, leading to more competition for the available clinic appointments. Consequently, patients may not have seen a psychiatrist for some time and their requirements may have changed. It is, however, also known1 that community patients who have not been reviewed recently or who have a long wait before their first assessment are more likely to present in crisis.
The diagnostic and second opinion function of the CRHTT is more prevalent when patients have been referred by the community team (67% reviewed, 47% medication changed) rather than on discharge from hospital (24% reviewed, 14% medication changed). This appears to largely reflect the fact that relatively few discharges were seen by the CRHTT psychiatrist because these patients had just received a full consultant-led discharge treatment plan. This may be another example of community service pressures leading to patient crises and thus engagement with alternative services – in this case inpatient care may be offering a second opinion service. The current separation of community and inpatient services will augment this effect as previously the patient would have been more likely to receive continuous care from the same consultant. This is an interesting view of current service configuration. The reduced continuity of care is often seen as a disadvantage but it does present an opportunity for a fresh evaluation of a patient’s diagnosis and medication by a different psychiatrist.
Longer lengths of stay with the CRHTT made psychiatric assessments more likely. It was particularly clear that discharge within a week made a psychiatric review unlikely. The proportion of community-referrals seen by a CRHTT psychiatrist could be increased to 83% if patients were to be seen within 24 hours. This figure is derived from the assumption that psychiatrists would then see the same proportion of both long and short stay patients. The residue would include those patients who refuse to engage with such an appointment.
It is interesting that chi-square statistical analysis suggests that the only influence on prescription change at the next appointment is whether the patient was seen by a CRHTT psychiatrist. It is not related to whether or not the CRHTT psychiatrist changed the medication. It is difficult to see why this should be the case unless the community psychiatrists consider the patients’ needs in more detail or are tempted to regain control after the referral to another psychiatrist.
In conclusion, the addition of psychiatric care to CRHTTs may be a valuable adjunct to the current pressures on community teams. The current trend to separate community, inpatient and CRHTT care is often cited as a disadvantage due to reduced continuity of care for patients. This project has drawn attention to the fact that it also offers opportunities for new teams to re-evaluate both diagnosis and treatment which offers patients the advantage of an internal second-opinion service. This advantage could be offered to more community-referred patients, albeit with more resources, by ensuring that they are assessed by the CRHTT psychiatrist within 24 hours.
Limitations
This is a small study conducted in a single CRHTT. It does, however, offer an indication of the evolving role of the CRHTT and its relationship to other services.
|
Competing Interests None Author Details PEARL OGAKU MBBS (FY2), Elizabeth Raybould Centre, Dartford, Kent DA2 6PB. ANNABEL MCDONALD MRCPsych (ST6), Elizabeth Raybould Centre, Dartford, Kent DA2 6PB. SHEEBA HAKEEM MRCPsych (ST6), Elizabeth Raybould Centre, Dartford, Kent DA2 6PB. M AAMER SARFRAZ PhD, Elizabeth Raybould Centre, Dartford, Kent DA2 6PB. CORRESPONDENCE: Dr. M Aamer Sarfraz, Consultant Psychiatrist & Director of Medical Education, Elizabeth Raybould Centre, Dartford, Kent DA2 6PB. Email: Aamer.Sarfraz@nhs.net |
References
- Gilburt H. Mental Health Under Pressure. Kings Fund Briefing 2015. [Online] Available at: https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/mental-health-under-pressure-nov15_0.pdf
- National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Healthy services and safer patients: links between patient suicide and features of mental health care providers. University of Manchester 2015. [Online] Available at: http://research.bmh.manchester.ac.uk/cmhs/research/centreforsuicideprevention/nci
- Imison C, Sonola L, Honeyman M, et al. The reconfiguration of clinical services: what is the evidence? Kings Fund 2014. [Online] Available at: https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/mental-health-under-pressure-nov15_0.pdf
- The Commission on Acute Adult Psychiatric Care. Improving acute inpatient psychiatric care for adults in England. Interim report. London: The Commission on Acute Adult Psychiatric Care. 2015. [Online] Available at: www.caapc.info/
- Royal College of Psychiatrists. ‘Trainee psychiatrist survey reveals mental health beds crisis’. 2014 [Online] Available at: www.rcpsych.ac.uk/mediacentre/pressreleases2014/traineesurvey.aspx
- Quirk A, Lelliot P. ‘What do we know about life on acute psychiatric wards in the UK? A review of the research evidence’. Social Science and Medicine 2001; 53: 1565-1574.
- Virtanen M, Vahtera J, Battey JB. et al. ‘Overcrowding in psychiatric wards and physical assaults on staff: data-linked longitudinal study’. British Journal of Psychiatry 2015; 198: 149-155.
- Johnson S. Crisis resolution and home treatment teams: an evolving model. Advances in Psychiatric treatment 2013; 19(2): 115-123.
- Dean C, Phillips J, Gadd E, et al. Comparison of community based service with hospital based service for people with acute, severe psychiatric illness. BMJ 1993; 307: 473-476.
- The 2010/11 National survey of Investment in Mental Health Services, s.l.: Department of Health. 2011.
- Mind. Crisis Services. 2013 [Online] Available at: http://mind.org.uk/information-support/guides-to-support-and-services/crisis-services/crht-crisis-teams/#.WHDwNoXXLIU
- Merriam-Webster, 2017. Merriam-Webster Inc., P.O. Box 281, Springfield, MA 01102.
- Funds cut for mental health trust in England. BBC, 2013. [Online] Available at: www.bbc.co.uk/news/health-25331644

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




