The health anxiety in medical students , a comparative study from Taif University : Medical student’s syndrome revisited.
Samiyah Siraj Althagafi, Maram Hassan AlSufyani, Ola Ahmed Shawky, Omayma Kamel Afifi, Naif Alomairi & Ibrahim Masoodi.
Cite this article as: BJMP 2019;12(1):a003
|
|
Abstract Background - Medical students sometimes develop fears related to the diseases they study during their pre-clinical and clinical years known as “Medical Student Syndrome” (MSS). |
Introduction
Medical Student Syndrome (MSS) is a unique type of hypochondriasis which specifically causes health anxiety related to the diseases medical students study during their medical training.1 However, this phenomenon does not translate into an increased number of consultations differentiating it from hypochondriasis.2 Nevertheless, the common denominator in both conditions is that the affected person persistently experiences the belief or fear of having severe disease, due to the misinterpretation of physical symptoms.3 The medical examination on multiple occasions does not identify medical conditions that fully account for the physical symptoms or the person’s concerns about the disease, making it a diagnosis of exclusion. Unfortunately, the fears frequently persist among medical students despite medical reassurance, affecting their concentration during their training.4
Earlier studies have shown a higher prevalence of MSS in various medical schools, but recent studies show a declining trend. While Howes et al5 demonstrated that 70% of medical students have groundless medical fears during their studies, Weck et al,6 on the contrary, recorded the prevalence of health anxiety only among 5-30 % of study participants. One of the reasons ascribed to this could be that earlier studies, showing a high prevalence of MSS, were uncontrolled. Also, age-matched peers were not used as controls in some studies, and no direct interviews had been conducted.7,8 Methodological issues in previous data have led to inaccurate interpretations and over-generalization of findings. For example, the high emotional disturbance in medical students resulted from comparisons made with the general population, rather than with other students of their age. 9-11
We were prompted to conduct this study because the magnitude of MSS is variable from region to region, and in this study we compared medical students with their peers, studying in different colleges of Taif University to avoid observational bias.
Methods
This study was carried out from September 2017 to June 2018 at the female campus of Taif University, Kingdom of Saudi Arabia (KSA) in medical (pre-clinical and clinical years) and non-medical colleges in accordance with research guidelines of the College of Medicine, Taif University, KSA.
Inclusion criteria
Age and gender-matched students were selected for inclusion in the study. These included:
1. Female medical students from the second to the sixth grades enrolled in the College of Medicine, Taif University, KSA.
2. Female non-medical students from first to fourth grades enrolled in colleges of Arts, Admin and Financial Sciences, Computer and Information Technology, Science and Islamic Law.
Exclusion criteria
Biology students were excluded due to the medical content of their courses. At the time of enrolment, permission for participant recruitment was obtained from the concerned faculty administrators.
The participants were approached in the common/study rooms or lecture halls. The students were informed of the voluntary nature of the participation and were randomly selected. They were not required to provide their names during completion of the questionnaire and were assured of confidentiality. The Hypochondria/Health Anxiety Questionnaire (HAQ), developed by the Obsessive Compulsive Centre of Los Angeles (http://ocdla.com/hypochondria-test), was used to collect the data. The questionnaire was translated into Arabic and underwent a revision in order to ensure compatibility with the original one. The questionnaire was not designed to provide a formal diagnosis but provided an indication as to whether or not the persons were exhibiting significant signs of the disease.
Results of this questionnaire were analyzed as under:
A) 1 to 3 test items checked: there is a low probability that the student has health anxiety, and it is unlikely that her concerns significantly impact his life.
B) 4 to 7 test items checked: there is a medium probability that she has health anxiety, and a moderately high amount of distress related to specific health-related thoughts. She spends more time than most people doing unnecessary behaviours related to these thoughts.
C) More than 7 test items checked: there is a high probability that she has health anxiety. She most likely has a significant amount of distress related to certain health-related obsessions, and likely spends a significant amount of time doing unnecessary compulsive and avoidant behaviours directly related to these obsessions.
Statistical methods
Data were statistically described regarding frequencies (number of cases) and valid percentages for categorical variables. The response of the two groups was analyzed by student t-test. P values less than 0.05 were considered to be statistically significant. All statistical calculations were done using computer program IBM SPSS (Statistical Package for the Social Science; IBM Corp, Armonk, NY, USA) release 21 for Microsoft Windows.
Results
400 students were included in the study. There were 200 medical students, and the other 200 students were from various non-medical colleges of Taif University (Colleges of Arts, Admin and Financial Sciences, Computer and Information Technology, Science and Islamic Law).
All participating students were females (100%), and the mean age of the medical students was 21 years (ranged from 19-22years). The mean age in the non-medical group was 20.5 years (ranged from 19-23 years).
All students in the non-medical colleges completed the HAQ while five students in the medical college (clinical years) did not complete it, so the data on 395 participants were finally analyzed.
According to the scaling criteria, this study showed that the overall prevalence of MSS among the total sample (medical and non-medical female students) was 16.2% (64 out 395 students). However, it was higher in the medical students (34 out of 195 students; 17.4%) than in the non-medical students (30 students out of 200; 15%) – see Table 1.
|
Non-medical students n=200 |
Medical students |
p value | ||
| Pre-clinical (95) | Clinical (100) | |||
| Age | 19-23 | 19-20 | 21-22 | |
| Medical student syndrome (MSS) | 30 (15%) | 20 (21.1%) | 14 (14%) | 0.22 |
| One visit to doctor | 33.3 % (10 /30) | 20 % (4/20) | 14.3 % (2/14) | 0.0043 |
| More than one visit to doctor | 40 % (4/10) | 25 % (1/4) | 0 % | 0.001 |
Table 1. The frequency of Medical Student Syndrome (MSS) among medical and non-medical students.
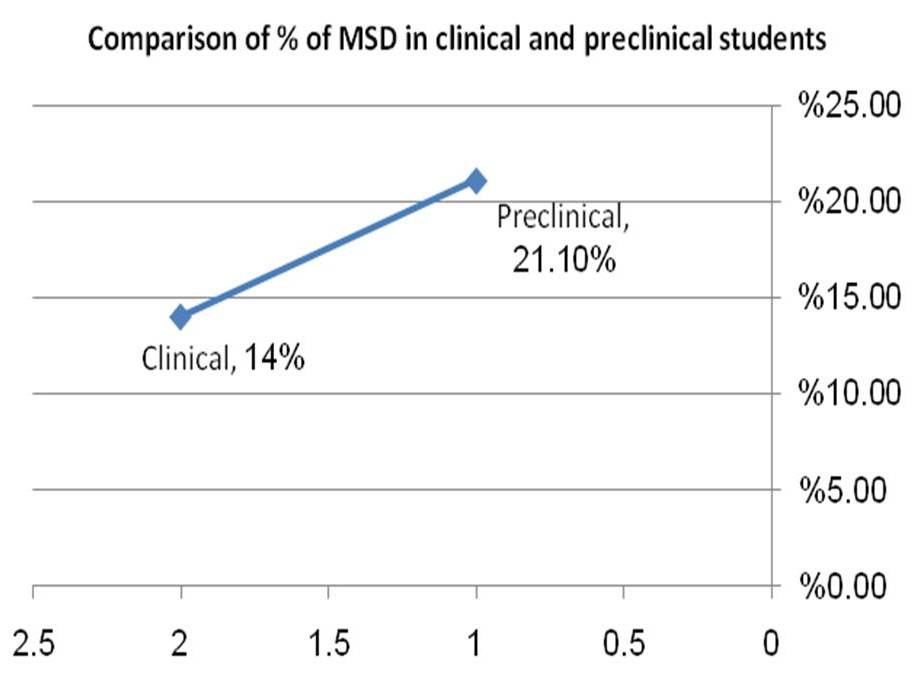
Figure 1. The difference of Medical Student Syndrome (MSS) between pre-clinical and clinical years (p=0.028).
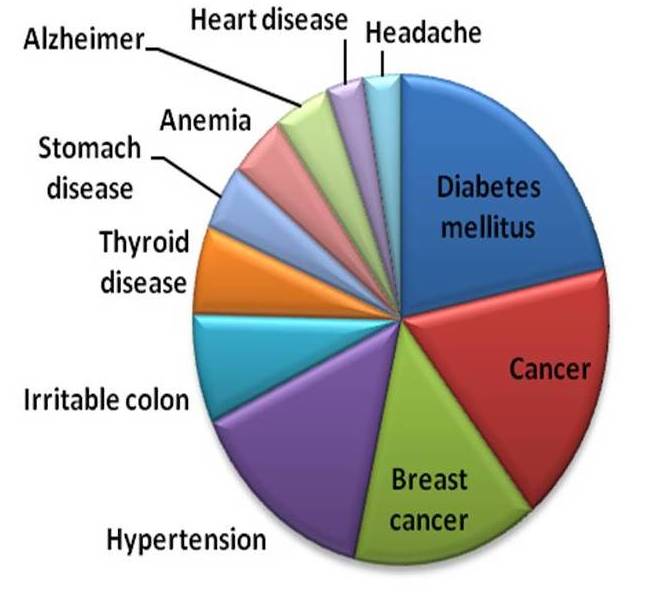
Figure 2. Fears related to diseases in the study cohort.
While comparing the response of the two groups by student t-test, there was no statistically significant difference between the responses obtained from medical and non-medical colleges (p=0.31). However, from the MSS diagnosed cases in the medical college, there was a significant difference between pre-clinical and clinical years – 21.1% vs 14% (p= 0.028) – see Figure 1.
Regarding the percentage of students who visited the doctors during the last year due to fears from disease, or medical condition, it was higher in the non-medical student's group than in the medical student's group with a significant difference observed (p=0.043).
The medical conditions that caused worry among medical and non-medical students were, diabetes mellitus followed by cancers especially breast cancer. The least worried diseases were headache and heart diseases – see Figure 2.
Regarding the percentage of students who consulted more than one doctor for the same medical concern, because of doubt about the previous doctor’s diagnosis and laboratory results, it was higher in the non-medical student's group compared to the medical student's group. The difference was significant (p=0.001).
The students with MSS in the total sample (of 395 students) were categorized according to the degree of probability into low, medium and high as shown in Figure 3.
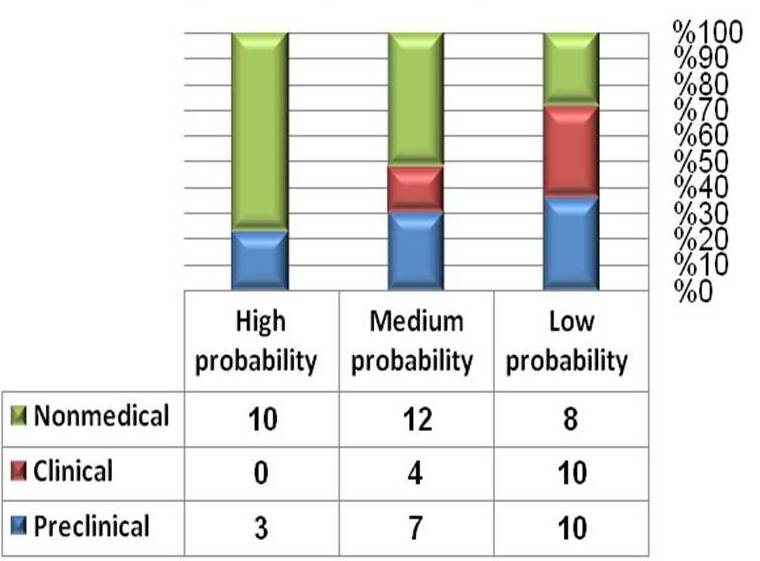
Figure 3. The probability of Medical Student Syndrome (MSS) among all groups compared to their non-medical peers.
Discussion
The unrealistic fears about illnesses recorded in this study among medical students were higher than their peers studying various non-medical courses at Taif University; however, the difference was not significant. The subgroup analysis revealed a correspondingly higher prevalence of health anxiety during pre-clinical years than clinical years as shown in Figure 1. Possibly during the pre-clinical years, students have an increased sense of body awareness and stress as demonstrated by Moss-Morris et al.7 The authors in the above study described this syndrome as a normal perceptual process and differentiated it from common hypochondriasis. Other researchers 8,12 as well affirmed this. Our results are in parallel with the finding of Azuri et al13 who recorded that first-year students visited a general practitioner (GP) or specialist more often than in other years. The authors in the above study suggested that the pre-clinical students` visits may be due to registering with a new doctor closer to university or due to necessary health checks before the beginning of their medical school. The dream content of pre-clinical medical students frequently involved a preoccupation with a personal illness of the heart, the eyes and the bowels in the above study.
Additionally, the fear of acquiring a future disease is a core feature of health anxiety, while fear of already having a disease is considered more central to the MSS.14 There is a number of instances where this syndrome manifests among students from time to time during their training. The students are even known to change their diagnosis depending upon their clinical rotation. For example, in a psychiatry rotation the student conceptualizes having schizophrenia and later shifts his or her diagnosis to Meniere's disease during an ear, nose and throat (ENT) rotation. The symptoms are thought to occur due to intensive exposure to knowledge affecting symptom perception and interpretation.15 The fact remains that the affected student is devoid of either. At times, the simple knowledge of the location of the appendix transforms the most harmless sensations in that region into symptoms of a serious threat.16 The students who study "frightening diseases" for the first time routinely experience intense delusions of having the disease, reflecting a temporary kind of hypochondriasis.17
In a study by Waterman et al18 it was observed that 80% of medical students conceptualize diagnoses ranging from tuberculosis to cancer while studying these diseases during training. This caused emotional distress and conflict in them. It was suggested that this phenomenon was present in approximately 70-80% of students in the study mentioned above. There may be multiple reasons for precipitation of this condition among medical students. The vastness of medical studies are undebatable, and medical schools cause students to experience a large amount of psychological pressure due to work required to grasp the subject matter, the stress of examinations, and the competitive environment.19
In this study, we compared medical students with the students of the same age and gender with the same cultural background in order to avoid any bias. Our results are in parallel with a more recent study, which compared three groups, medical students, non-medical students, and their peers who were not undergoing any academic course. The authors in the study mentioned above observed no significant differences between the groups on total scores in the questionnaires. However, when considering the individual components of the questionnaires, it was found that medical students were less aware of bodily changes and sensations than the other groups; nevertheless, they did not avoid seeking medical advice for any health-related fears.20
Regarding the percentage of students who visited doctors in the past 12 months due to fear of disease, it was observed in this study that the non-medical group had significantly higher visits to doctors compared to their peers studying in the medical college of the university. It is entirely possible that they had increased access to personal advice from peers, relatives, and various mentors. Of the various diseases, fear of diabetes mellitus was the highest, possibly due to a high prevalence of the disease in Saudi Arabia.21 Further, it is entirely possible that medical students subconsciously conceive these metabolic disorders as these are discussed in greater details during their courses.
MSS may lead to cyberchondria, a phenomenon of the public, seeking to diagnose themselves via the internet,11 which in turn may lead to hypochondriasis in any given student. Thus, it becomes imperative that students suffering from this disorder must be dealt with an empathetic approach and counselled properly after ruling out an organic cause of their illness. A step to circumvent it further would be that MSS must be thoroughly discussed among medical students during their training.
Limitation of the study
The drawback of this study is that that the questionnaire was translated from English into Arabic, and although it underwent a revision, there were no other formal tests such as linguistic and cultural validation to validate the translated version. Further, we believe that our focus was only on female students, and it is well known that females have better ability to cope up with anxiety and depression compared to males22,23 so the figures of MSS among male medical students needs to be studied as it may be different from what we reported in this female cohort.
Conclusion
In conclusion, the students who are suffering from MSS often overuse medical resources and outpatient’s services compared to others. Therefore, clinicians should be aware of these students, to avoid unnecessary procedures and treatments. However, it is vital that a proper evaluation is done before labelling a given student with MSS.
|
Competing Interests None declared Author Details SAMIYAH SIRAJ ALTHAGAFI, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. MARAM HASSAN ALSUFYANI, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. OLA AHMED SHAWKY, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. OMAYMA KAMEL AFIFI, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. NAIF ALOMAIRI, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. IBRAHIM MASOODI, Faculty of Medicine College of Medicine, Taif University, Saudi Arabia. CORRESPONDENCE: DR IBRAHIM MASOODI, College of Medicine, Taif Univeristy, Saudi Arabia. Email: ibrahimmasoodi@yahoo.co.in |
References
- Collier R. Imagined illnesses can cause real problems for medical students. CMAJ: Can Med Assoc J Journal del’Association Medicale Canadienne, 2008; 178(7): 820.
- Woods SM, Natterson J and Silverman J. Medical students’ disease: hypochondriasis in medical education. J Med Educ1966; 41(8): 785-790.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Text Revision. Washington, DC: American Psychiatric Association, 2000.
- Harding K, Skritskaya N, Doherty E, Fallon B. Advances in understanding illness anxiety. Current Psychiatry Reports. 2008; 10(4): 311-7.
- Howes OD, Salkovskis PM. Health anxiety in medical students. Lancet 1998; 351: 1332.
- Weck F, Richtberg S, Neng JM: Epidemiology of hypochondriasis and health anxiety: comparison of different diagnostic criteria. Curr Psychiatry Rev. 2014;10: 14.
- Moss-Morris R and Petrie KJ. Redefining medical students’disease to reduce morbidity. Med Educ, 2001; 35(8): 724–728: 15.
- Singh G, Hankins M, Weinman J. Does medical school cause health anxiety and worry in medical students? Medical Education. 2004; 38(5): 479-81.
- Firth J. Levels and sources of stress in medical students. 1986; BMJ. 292: 1177-1180.
- Heins, M, Fahey, S, Leiden, L. Perceived Stress in medical, law, and graduate students. Journal of Medical Education. 1984; 59(3): 169-79.
- Wickham, S. The perils of cyberchondria. Practising Midwife. 2009; 12(2): 34.
- Warwick HM and Salkovskis PM. Hypochondriasis. Behav Res Ther. 1990;28 (2): 105-17.
- Azuri J, Ackshota N, Vinker S. Reassuring the medical students’ disease: Health-related anxiety among medical students. Medical Teacher. 2010; 32(7): 270-275.
- Robert E. Brady and Jeffrey M. A behavioural test of contamination fear in excessive health anxiety) J. Behav. Ther. & Exp. Psychiat. 2014;45: 122-127.
- Janssens T, Verleden G, De Peuter S, Van Diest I, Van den Bergh O. Inaccurate perception of asthma symptoms: a cognitive-affective framework and implications for asthma treatment. Clin Psychol Rev. 2009 Jun;29(4): 317-27.
- Walton, and Lincoln G. Why Worry? Philadelphia, PA, US: JB Lippincott Company, 1908; pp275.
- Baars, and Bernard J. In the Theater of Consciousness: The Workspace of the Mind. Oxford University Press US. 2001.
- Waterman LZ, and Weinman JA. Medical student syndrome: fact or fiction? A cross-sectional study. J Royal Society Medicine Open, 2014; 5(2): 1-9.
- Dyrbye L, Thomas M, Shanafelt T. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Academic Medicine. 2006; 81(4): 354-73.
- Mechanic D. Social psychologic factors affecting the presentation of bodily complaints. New England Journal of Medicine. 1972; 286(21): 1132-9.
- Khalid Al-Rubeaan, Hamad Al-Manaa, Tawfik Khoja, et al. The Saudi Abnormal Glucose Metabolism and Diabetes Impact Study (SAUDI-DM) Ann Saudi Med. 2014 Nov-Dec; 34(6): 465-475.
- Sharma B, Wavare R. Academic stress due to depression among medical and para-medical students in an Indian medical college: Health initiatives cross-sectional study. J Health Sci 2013; 3(5): 29-38.
- Khan MS, Mahmood S, Badshah A, Ali SU, Jamal Y. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J Pak Med Assoc 2006; 56(12): 583.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




