Impact of diabetes education and peer support group on the metabolic parameters of patients with Diabetes Mellitus (Type 1 and Type 2)
Issac Sachmechi, Aileen Wang, Paul Kim, David Reich, Hildegarde Payne and Vincent Bryan Salvador
Cite this article as: BJMP 2013;6(4):a635
|
|
Abstract Aim This study was undertaken to investigate the effect of diabetes education (DE) alone versus diabetes education plus peer support group (DE+PS) in improving metabolic parameters in patients with diabetes mellitus (DM). Abbreviations: DM – diabetes mellitus, HB A1C - Hemoglobin A1C (HB A1C), BMI - body mass index (kg/m2), SBP - systolic blood pressure, TC - total cholesterol, HDL-C - HDL cholesterol, LDL-C - LDL cholesterol, TG - triglycerides, ADA - American Diabetes Association |
Introduction
Population-based studies indicated that diabetes remains as a nationwide epidemic that continues to grow tremendously affecting 25.8 million people or 8.3% of the US population.1 This number is expected to reach 68 million or 25% of the population by 20302 as incidence of obesity is rising.3
The American Diabetes Association (ADA) recognizes diabetes education (DE) as an essential part of comprehensive care for patients with diabetes mellitus and recommends assessing self-management skills and knowledge at least annually in addition to participation in DE.4 With the objective of improving the quality of life and reducing the disease burden, the ADA and the U.S. Department of Health and Human Services through its Healthy People 2020 program have emphasized three key components for effective disease management planning: regular medical care, self-management education and ongoing diabetes support.5,6
The hallmark of preventing the chronic complications of diabetes lies in optimizing metabolic parameters such as glycaemic control, blood pressure, weight and lipid profile. Pharmacologic intervention can only do so much in achieving treatment goals. It should be complemented with appropriate DE emphasizing dietary control, physical activity and strict medication adherence.7,8 Adequate glycaemic control is clinically important because a percentile reduction in mean HbA1C is associated with a 21% reduction in diabetes-related death risk, 14% reduction in heart attacks and 37% reduction in microvascular complications.9
Diabetes self-management (DSM) education programs are valuable strategy for improving health behaviours which have significant impact on metabolic parameters.10 This is supported by chronic care model that is based on the notion that improving the health of patients with chronic diseases depends on a number of factors that include patients’ knowledge about their disease, daily practice of self-management techniques and healthy behaviors.11,12,13
A systematic review by Norris et al. has shown that DSM training confers positive effect on patients’ knowledge about diabetes, blood glucose monitoring, and importance of dietary practices and glycaemic control.14 In another retrospective observational study, evidence has suggested that participation in a multifactorial diabetes health education significantly improved glycaemic and lipid levels in the short term.10
Diabetes education/support group provides a comprehensive patient education, fosters a sense of community, and engages the patients to become active part of a team managing their diabetes. The diabetes support group at Queens Hospital Centre provides services to a diverse population from different socioeconomic backgrounds and is offered to any patients with diabetes. It is facilitated by certified diabetes nurse educators in the hospital and in the clinic. Patients meet once a month per session and are provided education in self-management of diabetes, education in medication, diet, lifestyle modifications, regular exercise, weight management and translation in their respective languages, if needed.
Few researches have been conducted comparing the efficacy of DE and combination of diabetes education and peer support group (DE+PS) in improving the metabolic parameters of patients with DM. In patients with DM, the primary objective of this study was to assess the clinical impact of DE and combined DE+PS group on metabolic parameters such as lowering HbA1C, reducing weight or BMI, controlling blood pressure, and improving lipid profile.
Methods
The study subjects were identified through retrospective review of electronic medical records of adult patients aged more than 18 years old with diabetes and being treated at the Diabetes Centre and/or Primary Care Clinic of Queens Hospital Centre, Jamaica, New York from January 01, 2007 to June 01, 2011. A total of 188 study subjects were selected and assigned to three groups: (1) control group (n=62), who received primary care only, (2) DE group (n=63), who received diabetes teaching from DM nurse educator in addition to primary care, and (3) DE+PS group (n=63), who received both diabetes education and attended at least 2 or more sessions of peer support group in addition to primary care. The subjects in control group, education group, education plus peer support group were matched on age, sex, weight and BMI. Considering the data availability, the duration of follow up measured in each group varied; the control group was followed up for 8 months, the DE group for 13 months and the DE+PS group for 19 months. The changes from mean baseline to the third month, sixth month and final follow up period were calculated for the following metabolic parameters: HbA1C, weight, BMI, SBP, TC, HDL-C, LDL-C and TG-C. T sample T-test was used to compare statistical differences in the mean changes in the metabolic parameters in each group from baseline to follow up period. All data management and statistical analyses were conducted with MiniTab version 14. A p-value of less than 0.05 is considered statistically significant.
Results
Among the 188 study subjects included in our study between ages 20 to 88 years with mean age of 60, the predominant gender was female (n=132, 70%). African American makes up the majority (n=74, 39%), followed by Asian (n=40, 21%), Caucasian (n=34, 18%), Hispanic (n=22, 12%) and Indian (n=18, 10%). Majority of our patients with DM have concurrent hypertension (91%), hyperlipidemia (90%), and obesity (47%). See Table 1 for baseline demographics.
| Table 1. Baseline demographic characteristics of the study population | |||
| Control [C] N=62 |
Diabetes Education [DE] N=63 |
Diabetes Education + Peer support [DE+PS] N=63 |
|
| Baseline Characteristics | |||
| Age range (years) [median] | 32-76 [61] | 20-88 [58] | 26-86 [62] |
| Sex-male [N (%)] | 22 (35) | 20 (32) | 14 (22) |
| Race | |||
| African American | 31 (50) | 26 (41) | 17 (27) |
| White | 11 (17) | 23 (37) | 0 (0) |
| Indian | 18 (29) | 0 (0) | 0 (0) |
| Asian | 1 (2) | 10 (16) | 29 (46) |
| Hispanic | 1 (2) | 4 (6) | 17 (27) |
| Comorbidities [N (%)] | |||
| Hypertension# | 54 (87) | 59 (94) | 58 (92) |
| Hyperlipidemia¥ | 56 (90) | 61 (97) | 53 (84) |
| Obesity* | 29 (47) | 29 (46) | 31 (49) |
| Active cigarette smoker | 6 (10) | 5 (8) | 1 (2) |
# Hypertension is defined as mean systolic blood pressure > 140 mmHg and/or diastolic > 90 mmHg measured on two separate occasions. These patients have either hypertension diagnosed prior to or after diagnosis of DM.
¥ Hyperlipidemia is defined as LDL > 100 mg/dl in patients with diabetes and diagnosis hyperlipidemia could be before or after diagnosis of DM.
* Obesity is defined as body mass index (BMI) of at least 30 kg/m2 or greater.
The group analysis showed that the DE group had a statistically significant decrease in mean HbA1C (mean change: -0.78%, p=0.013), TC (mean change: -16.89 mg/dL, p=0.01) and LDL-C (mean change: -11.75 mg/dL, p=0.04) from baseline to final follow up (see Table 2). The DE group had non-significant mean weight gain of 2.17 pounds and BMI of 0.52 kg/m2.
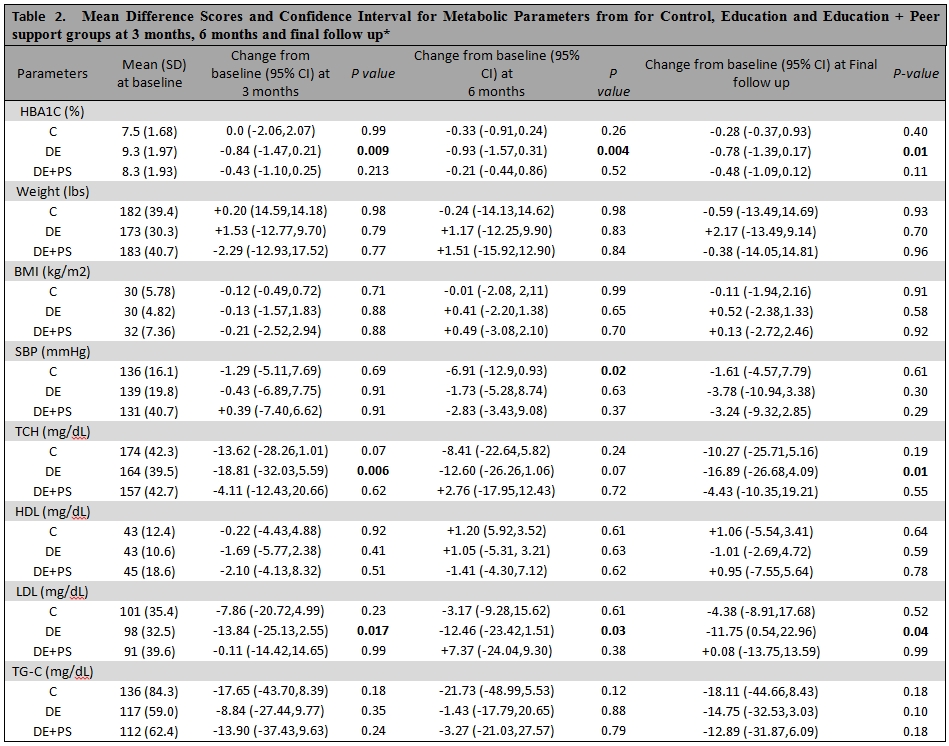
* Final follow up varies for the three groups. 8 months for control (C), 13 months for education (DE) group and 19 months for education plus peer support (DE+PS) group
Although DE+PS group were observed to have decreased in mean HbA1C (-0.48%), weight (-0.38 pounds), SBP (-3.24 mmHg), TC (-4.43 mg/dL) and TG-C (-12.89 mg/dL) and increased in HDL-C (+095 mg/dL), they were not statistically significant from initial to final follow up period. There were greater improvements in HbA1C and SBP from baseline to final follow up in DE+PS group compared to the control group. Only the control and DE+PS groups showed a decrease in weight from initial to final follow up.
Between the two intervention arms, the DE group exhibited greater reduction compared to DE+PS group in mean HbA1C (-0.78 vs. -0.48%), SBP (-3.78 vs. -3.24 mmHg), TC (-16.89 vs. -4.43 mg/dL), LDL-C (-11.75 vs. +0.08 mg/dL) and TG-C (-14.75 vs. -12.89 mg/dL).
Discussion
Our results suggested that among patients with DM, the subjects who participated in DE exhibited significant reduction in baseline HbA1C, TC and LDL-C compared to control. Furthermore, the significant impact of DE alone on optimizing control of HbA1C and LDL-C appeared to persist through time. In addition patients who received DE+PS also demonstrated moderate improvement in HbA1C, SBP, TC and TG-C and HDL-C even though they were not statistically significant on final follow up. It must be noted that the baseline mean HbA1Cs were higher in both interventions DE and DE+PS groups compared to control group and this may be associated with greater reduction in HbA1C in the intervention groups and may skew the finding. Our study results showed that DE group had greater percentage reduction in HbA1C (9%) compared to DE+PS group (5%) from baseline to the first follow up. The average change in HbA1C and LDL-C levels recorded in our study is similar to what has been reported in a previous study which showed significantly greater improvement in mean glycaemic levels and LDL-C levels in patients who participated in DE.10
However our findings are in stark contrast to a previous study that showed that DE+PS intervention has led to substantially greater weight reduction and improvement in HbA1C at second month post-intervention compared to education and control group.15 This difference may be accounted for by the effect of sample size and the duration of follow up. The DE+PS group in our study included twice the number of patients being sampled compared to previous study (63 patients vs. 32 patients), and longer duration of follow up (19 months vs. 4 months)15. These differences are significant as they can influence the data trend.
In general, all groups had improvement in HbA1C, TC, TG-C levels, and SBP (though not significant). Only control and DE+PS groups had weight reduction and DE group had weight increase. Although the DE+PS group had improvement in most of the metabolic parameters they were not statistically significant throughout the entire follow up period compared to DE group. This scenario might be attributed to retrospective nature of the study, possible non-compliance of patients to medications, differences in duration of follow up between groups, and limited number of patients sampled thus hindering the appreciation of potential significant effect. The statistically significant differences in baseline HB A1C among the three groups could also explain the differing magnitude of change from baseline; DE group had higher baseline HbA1C compared to control group (9.3 vs. 7.5%; p=0.00) allowing for a greater change from baseline value. Similarly in DE+PS group, baseline HbA1C was considered statistically significant compared to control group (8.3 vs. 7.5%, p=0.018).
A previous randomized controlled trial assessing the effect of peer support on patients with type 2 diabetes with a 2-year follow up demonstrated no significant differences in HbA1C (-0.08%, 95% CI -0.35% to 0.18%), SBP (-3.9 mmHg, -8.9 to 1.1 mmHg) and TC (-0.03 mmol/l, -0.28 to 0.22 mmol/l).16 It was suggested that the effect of DSM education on glycaemic control is greatest in the short-term and progressively attenuated over time and this may suggest that learned behaviour changes with time.17,18 However, the result of the present study showed a persistently significant beneficial effect on HbA1C and LDL-C from the earliest follow up until the final month for patients receiving DE alone.
Previous meta-analysis of randomized trials of DSM education programs by Norris and colleagues (2002) demonstrated the beneficial effect of DE with estimated effect on glycaemic control (HbA1C) at -0.76% (95% CI: 0.34,1.18) compared to control immediately after the intervention.17 However, the findings of the present study on the effect of peer education are in direct contrast with the results of the randomized trial using the Project Dulce model of peer-led education showing significant improvement from baseline to the tenth month of follow-up in HB A1C (-1.5%, p=0.01), TC (-7.2 mg/dl, p=0.04), HDL-C (+1.6 mg/dl, p=0.01) and LDL-C (-8.1 mg/dl, p=0.02).19 This could be accounted for the different baseline values of the metabolic parameters in the present study, thus creating a bias in the magnitude of change.
It has been suggested that the most effective peer support model includes both peer support and a structured educational program. The emphasis on peer support is based on the recognition that people living with chronic illness can share their knowledge and experiences to one another.20 It has been observed that participants in peer support groups were not interested in the topic of diabetes itself but on the effect and meaning of the disease on the lives of the patients.21
There are a number of limitations to be taken into consideration when interpreting the results of our study. Since our study is a retrospective review of medical records, the data collection was limited to availability of the required clinical data. Some parameters were not possible to obtain on a consistently uniform time frame. This resulted in varying mean duration for the 3 study groups (8 months for control group, 13 months for DE and 19 months DE+PS group). Because of unavailability of some of the clinical parameters at a specific time frame, there were variables missing on the earlier follow-ups. Our study also examined the effect of the intervention over a relatively short time. A longer-term study is necessary to determine if the intervention has lasting impact on improving the metabolic parameters, uplifting the quality of life and preventing morbidity and mortality from diabetes. The limited sample size could also be important factor that may influence the generalizability of the data. The differing baseline values in the metabolic parameters could have blunted the appreciation of possible significant improvement in the metabolic parameters in the DE+PS group. Other confounding factors that were not analysed in the present study and could have affected the results include the use of insulin regimen among the different groups, initiation of additional oral hypoglycemic agents, medication adherence by the patients and adjustment by physicians, and whether the patients were seen by endocrinologists or not.
The present study suggested that participation in DE may assist with optimizing HbA1C, TC and LDL-C. The DE group had improvement in glycaemic control and other metabolic parameters. The significant metabolic improvement gained from DE appeared to be sustained over time. However, participation in both DE+PS showed relative improvement but not significant as it is likely due to confounding different baseline metabolic parameter and duration being compared. Our findings underscore the importance of DE as part of the treatment plan for patients with DM. The addition of peer support group may or may not contribute to significant improvement of metabolic parameters.
|
Acknowledgements The authors would like to extend their gratitude to: Nayab Bakshi, Edan Elias and Dorota Pazdrowska for assistance on data recording. Competing Interests None declared Author Details ISSAC SACHMECHI, M.D., FACP, FACE, Department of Medicine, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, Jamaica, NY, USA 11432. AILEEN WANG, M.D., Department of Medicine, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, Jamaica, NY, USA 11432. PAUL KIM, M.D., FACE, Department of Medicine, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, Jamaica, NY, USA 11432. DAVID REICH, M.D., FACE, Department of Medicine, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, Jamaica, NY, USA 11432. HILDEGARDE PAYNE, R.N., CDE, Diabetes Clinic, Queens Hospital Center, Jamaica, NY, USA 11432. VINCENT BRYAN SALVADOR, M.D., Department of Medicine, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, Jamaica, NY, USA 11432. CORRESPONDENCE: VINCENT BRYAN SALVADOR, Icahn School of Medicine at Mt. Sinai/Queens Hospital Center, 82-68 164th Street, Jamaica, NY, USA 11432. Email: docvincesalvador@aol.com |
References
- Centres for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011[Internet]. Atlanta (GA);2011. Available from: http//www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.
- Boyle JP, Thompson TJ, Gregg EW, et al. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modelling of incidence, mortality and prediabetes prevalence. Popul Health Metr. 2010; 8:29.
- S. Wild, G Roglic, A. Green, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27 (5);2004; 1047-1053.
- American Diabetes Association. Standards of medical care for patients with diabetes mellitus (position statement). Diabetes Care 2001;24 (Suppl 1):S33-43.
- Healthy People.gov. Healthy People 2020:goals and objectives-diabetes [Internet]. Washington (DC):Department of Health and Human Services; 2011. Available from: http://healthypeople.gov/2020/topicsobjectives 2020/overview.aspx?topicid=8.
- American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care. 2011;34 (Suppl 1):S11-8
- Gaede P, Lund-Andersen H, PArving H-H, et al. Effect of multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580-591.
- Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, et al. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death and microvascular events in type 2 diabetes: meta-analysis of randomized controlled trials. BMJ 2011;343:d4169.
- Stratton IM, Adler AI, Neil JA, et al. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35):prospective observational study. BMJ 2000;321(7258):405-12.
- Roblin DW, Ntekop E, Becker ER. Improved intermediate clinical outcomes from participation in a diabetes health education program. J Ambulatory Care Manage 2007; 30(1);64-73.
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002a. 288(14), 1775-1779.
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness:the chronic care model, part 2. JAMA 2002b, 288(15),1909-1914.
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Quarterly 1996, 74(4), 511-544.
- Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes. A systematic review of randomized controlled trials. Diabetes Care 2011, 24(3),561-587.
- Wilson W. Pratt C. The impact of diabetes education and peer support upon weight and glycaemic control of elderly persons with noninsulin dependent diabetes mellitus (NIDDM).Am J Public Health May 1987; 77(5),634-635.
- Smith SM, Paul G, Kelly A, Whitford DL, et al. Peer support for patients with type 2 diabetes: cluster randomized controlled trial. BMJ 2011;342:d715.
- Norris SL, Lau JS, Schmid CH, et al. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycaemic control. Diabetes Care 2002; 25(7),1159-1171.
- Brown S. Meta-analysis of diabetes patient education research: variation in intervention effects across studies. Res Nurs Health 1992;15:409-419.
- Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, et al. Peer-led diabetes education programs in high-risk Mexican Americans improve glycaemic control compared with standard approaches. Diabetes Care 2011;34:1926-1931.
- Heisler M. Overview of peer support models to improve diabetes self-management and clinical outcomes. Diabetes Spectrum 2007;20(4):214-221.
- Rugh D. Design of a rural diabetes self-directed care program. Soc Work Health Care 2011;50(10):775-786.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




