Isolated Arthroscopic Lateral Patella Retinaculum Release for Anterior Knee Pain – Is it worth it?
Sultan N Qasim, Kimberly Lammin and Phillip Edge
Cite this article as: BJMP 2016;9(1):a908
|
|
Abstract Introduction: ‘Anterior Knee Pain’ is a common presentation in all age groups and aetiology is not fully understood. Arthroscopic Lateral Patellar Retinaculum Release has been a commonly performed procedure to treat anterior knee pain with variable results. Methods: We performed a retrospective review of all the patients who underwent isolated arthroscopic lateral patellar retinaculum release under a single surgeon between July 2007 and July 2010. Exclusion criteria included significant patellar instability, severe mal alignment, and additional procedures including meniscal repair/excision or medial patella plication. Primary outcome measure was improvement in post procedure Oxford Knee Score. Results: There was significant improvement in OKS, in particular ability to kneel and climb stairs, associated with a high degree of arthritis in patellofemoral articulation and post-operative physiotherapy. However, OKS components lost this significance with tibiofemoral articulation wear of Outerbridge grade 3 or higher. The procedure had a high mean satisfaction score of 8.2 (range 4 to 10) and 32 of 36 patients would have the procedure again if need be. Conclusions: Isolated Patella Retinaculum release can be effective for anterior knee pain without significant instability or mal-alignment. It particularly improves patients’ ability to kneel and climb stairs giving a high satisfaction score - grade of wear of patellofemoral cartilage being most important factor. Post-operative physiotherapy further augments the good results. However it has no significant value in the presence of advanced tibiofemoral degeneration irrespective of state of patellofemoral articulation. Keywords: Anterior Knee Pain, Arthroscopic, Patella, Lateral ReleaseAbbreviations: OKS - Oxford Knee Score |
Introduction
Anterior knee pain or patellofemoral pain is a common clinical presentation especially in females. It is a challenging clinical problem. The specific cause can be difficult to diagnose as the aetiology remains poorly understood and there are various pathologic entities that can result in pain in the anterior aspect of knee.
Multiple surgical options have been used to treat the condition. Lateral retinacular release is one of these options and has been used to treat anterior knee pain with variable results1-5. The aim of this study was to assess isolated patella lateral retinaculum release as a treatment for anterior knee pain.
Materials and Methods
We performed a retrospective review of all the patients who underwent isolated arthroscopic lateral patella retinacular release under a single surgeon between July 2007 and July 2010. Exclusion criteria included significant patellar instability and severe mal-alignment on both radiological and clinical assessment and additional procedures including cartilage debridement, meniscal tear repair/excision or patella stabilization.
Data was collected from case notes (demographics, pre-operative and intra-operative findings and any post-operative complications), archived radiographs and postal questionnaires including pre and post procedure Oxford Knee Score (OKS), as well as patient satisfaction. Patient satisfaction questions included a grading of satisfaction of 1(completely dissatisfied) - 10 (completely satisfied) and whether patient would reconsider the procedure if given the choice again.
Independent factors assessed were age, sex, tight lateral retinaculum, osteoarthritic x-ray changes of all compartments, intraoperative findings of grade of arthritis and lateral subluxation and postoperative physiotherapy. The primary outcome assessed was patient reported outcome measures, including the improvement in post procedure OKS and patient satisfaction scores. SPSS Version 20 was used for analysis.
Preoperative and Postoperative OKS – total and components - were compared using Wilcoxon Signed Rank Test. The Mann Whitney U test was used for nominal data and Kruskal-Wallis test was used for continuous data for total OKS. Individual OKS components compared were ability to kneel and ability to climb stairs - more representative of patellofemoral joint.
Results
59 patients were identified with male to female ratio of 1:1.5. The mean age was 58.7 (range 25 to 77). 40 patients (67%) returned completed forms. Four patients had further surgery; three total knee replacement and one subsequent arthroscopic procedure for meniscal tears. These patients were excluded from the study. Four patients had bilateral procedures. Therefore after the exclusions for further surgery and those who failed to return completed forms 36 patients were included, on whom 40 procedures had been performed. Changes of osteoarthritis - graded according to Kellgren and Lawrence system - on the medial and lateral facets of the patella were noted on preoperative Merchant views (Table 1) and the tibiofemoral compartment as well.
Table 1 – Pre-Operative Radiographic grades of Patellofemoral change
| Medial Facet | Lateral Facet | |||
| Grade | Frequency | % | Frequency | % |
| 0 | 2 | 5 | 1 | 2.5 |
| 1 | 6 | 15 | 4 | 10 |
| 2 | 15 | 37.5 | 13 | 32.5 |
| 3 | 16 | 40 | 15 | 37.5 |
| 4 | 1 | 2.5 | 7 | 17.5 |
| Total | 40 | 100 | 40 | 100 |
All patients had undergone standardized preoperative physiotherapy regimen with no significant benefit. Two had, had intra-articular hyaluronic acid injection with no benefit.
All procedures were performed by a single surgeon (PE) and intraoperative findings of cartilage Outerbridge grade were noted in all compartments. Closed lateral retinacular release was performed with Smiley’s knife from just below lower end up to the upper border of patella.
Mean follow up duration was 20.43 months +/- 10.64. Patients were divided into three groups of follow up durations. 6-12 months had 6, 12-18months had 18 and >18months had 16 cases. The best results were in 12-18 month follow up but no statistically significant difference was found between different groups. There was no significant difference in age and gender distribution amongst different durations of follow up. Also there was no significant difference in age, gender and different durations of follow up between responders and non-responders of the questionnaire. There were no reported postoperative complications.
24(60%) underwent post-operative physiotherapy. The mean OKS improved from 23.05 (range11-40) to 35.30 (range14-48) [p value <0.0001]. Individual components of OKS, particularly ability to climb stairs and ability to kneel, also showed statistically significant improvements (Figure 1, Figure 2).
Fig 1 – OKS – ability to climb stairs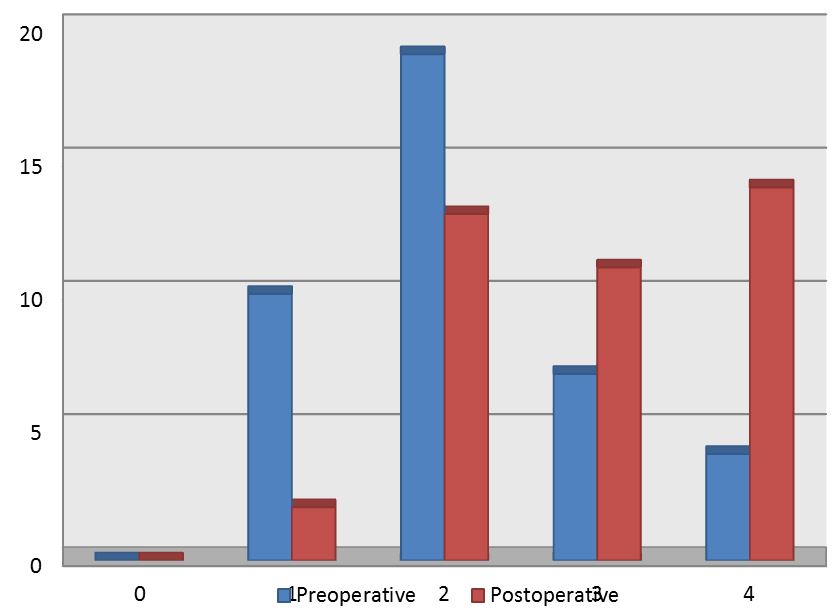
Fig 2 – OKS – ability to kneel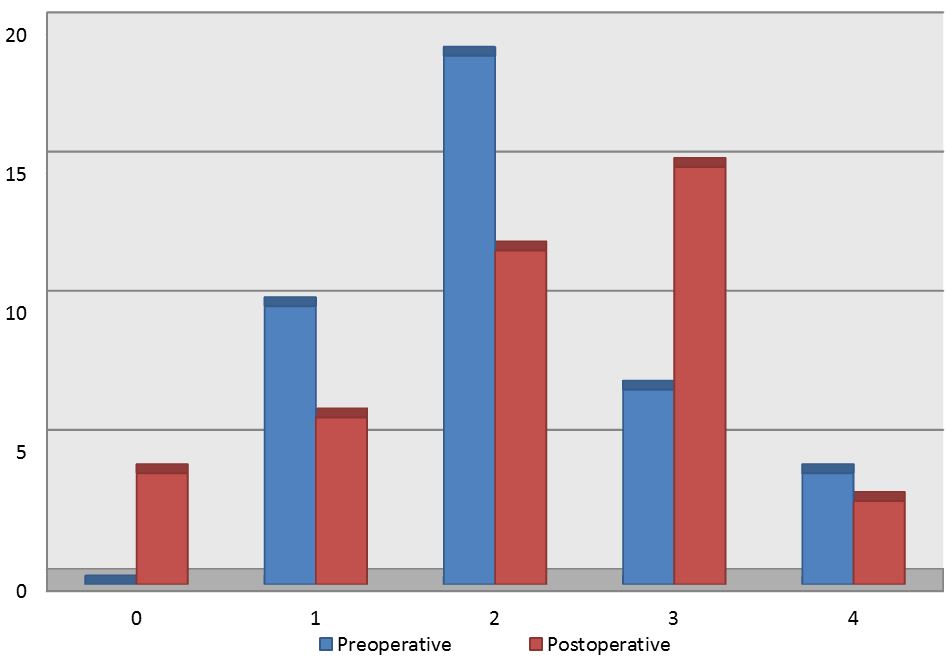
Univariate analysis showed improvement of total OKS and OKS for ability to kneel were significantly associated with higher grade of radiographic lateral patellofemoral joint wear (p value 0.025 and 0.042 respectively) and postoperative physiotherapy (p value 0.018 and 0.003) and improvement in OKS for ability to climb stairs was significantly associated with higher grade cartilage wear, noted intraoperatively, for trochlea (p value 0.042) and patella (p value 0.022).
However the OKS components lost this significance if there was Outerbridge Grade 3 or more wear in tibiofemoral articulation.
The procedure had a high mean satisfaction score of 8.2 (range 4 to 10), and 32 of 36 patients would have the procedure again if needed.
Discussion
Anterior Knee pain or patella pain syndrome is a very common clinical problem faced by orthopaedic surgeons. However the aetiology remains poorly understood. Mori et al6identified evidence of degenerative neuropathy in 29 out of 35 histologically examined specimens of resected lateral retinaculum; thus suggesting it may originate in the lateral retinaculum. Lateral Retinacular release would denervate this tissue producing symptomatic relief. Osterneier et al7 measured patellofemoral contact pressures and kinematics using fresh-frozen cadaver specimens both before and after lateral release. They concluded that release could decrease pressure on the lateral patella facet in flexion but did not stabilize the patella or medialise patella tracking. This possibly explains our finding of improvement with lateral patellofemoral joint wear.
Arthroscopic lateral release remains a controversial topic because of lack of well-designed randomised studies. Fulkerson and Shea8 suggested that knees showing lateral patellar tilt without subluxation were more likely to benefit from a lateral release in the absence of grade III or grade IV changes in the articular cartilage. Korkala et al9 showed that a lateral release tended to improve symptoms in patients with grade II to grade IV chondromalacia. Our findings concur that greater the patellofemoral articulation cartilage wear the more significant the improvement.
Lodhi et al10 performed a prospective study of elderly patients with patellofemoral osteoarthritis and pain which conservative management had failed to improve and concluded that the procedure improves function and provides significant pain relief successfully deferring need for arthroplasty; therefore they recommended the procedure in middle aged to elderly patients with symptomatic patellofemoral osteoarthritis.
Twaddle and Parkinson11 suggested lateral release to be an effective, reliable and durable procedure in ‘carefully selected patients’ through their retrospective study.
Our study has deficiencies regarding single surgeon series and retrospective review. However it reflects some of the findings from previous studies suggesting that it is an effective procedure to improve symptoms associated with cartilage changes in patellofemoral articulation without significant tibiofemoral joint osteoarthritis. Further well designed randomized controlled trials are needed to give a more definitive answer.
Conclusion
Isolated lateral patella retinacular release can be effective for anterior knee pain in carefully selected patients, (without significant instability or mal-alignment, with high patellofemoral but low tibiofemoral wear), who have failed conservative management. It particularly improves patients’ ability to kneel and climb stairs, giving a high satisfaction score. The grade of wear of patellofemoral cartilage is the most significant factor in determining this, with post-operative physiotherapy further augmenting the good results.
|
Competing Interests None declared Author Details SULTAN QASIM, FRCS(TR&ORTH), Univeristy Hospitals of Leicester NHS Trust, UK. KIMBERLY LAMMIN, FRCS(TR&ORTH), Univeristy Hospitals of Leicester NHS Trust, UK. PHILLIP EDGE, FCS(SA), Bedford Hospital, UK. CORRESPONDENCE: SULTAN QASIM, Univeristy Hospitals of Leicester NHS Trust, Infirmary Square, Leicester. LE1 5WW. UK Email: drsnqasim@gmail.com |
References
- Larson RL, Cabaud HE, Slocum DB, et al. The patelar compression syndrome: surgical treatment by lateral retinacular release. Clin Orthop 1978;34:158-67.
- Aglietti P, Pisaneschi A, Buzzi R, Gaudenzi A, Allegra M. Arthroscopic lateral
- release for patellar pain or instability. Arthroscopy 1989;5:176-83.
- Christensen F, Søballe K, Snerum L. Treatment of chondromalacia patellae by lateral retinaclar release of the patella. Clin Orthop 1988;234:145-7.
- Vadivelu R, Ratnam SA, Margetts MJ (2004) Functional and clinical outcome following arthroscopy and lateral release in patella disorders – A Prospective Clinical Study.J Bone Joint Surg Br 2004 vol. 86-B no. SUPP III 254
- Alvarez-Vega M, Ferrero-Manzanal F, Iglesias-Colao R, Murcia-Mazón A (2004) Evaluation of knee retinacular lateral releases using an arthroscopic technique.J Bone Joint Surg Br 2004 vol. 86-B no. SUPP III 254
- Mori Y, Fujimoto A, Okumo H, Kuroki Y. Lateral retinaculum release in adolescent patellofemoral disorders: its relationship to peripheral nerve injury in the lateral retinaculum. Bull Hosp Jt Dis Orthop Inst 1991;51:218-29.
- Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C (2007) Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007 May;15(5):547-54.
- Fulkerson JP, Shea KP. Disorders of patellofemoral alignment. J Bone Joint Surg
- [Am] 1990;72-A:1424-9.
- Korkala OL, Isotalo TM, Lavonius MI, Niskanen RO. Outcome and clinical signs of arthroscopically graded patellar chondromalacia with or without lateral release. Ann Chir Gynaecol 1995;84:276-9.
- Lodhi Y, Durve K, El Shazly M (2010) Lateral release in middle aged to elderly population with patellofemoral osteoarthritis; Long-term Follow-up. J Bone Joint Surg Br 2010 vol. 92-B no. SUPP IV 539
- Twaddle BC, Parkinson S (2005) Lateral release for Isolated Lateral Facet OteoarthritisJ Bone Joint Surg Br 2005 vol. 87-B no. SUPP I 24-25

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




