Malignant Syphilis as an Initial Presentation of Underlying HIV Infection: A Case report
Ashok R Devkota, Rabindra Ghimire, Mirela Sam and Oo Aung
Cite this article as: BJMP 2015;8(2):a816
|
|
Abstract There is a higher rate of HIV coinfection among men who have sex with men (MSM) infected with syphilis. HIV positive patients present more often with secondary syphilis and disease course is more aggressive. Here we present a patient, with diffuse papulo-nodular and ulcerative skin lesion and newly diagnosed human immunodeficiency virus. Biopsy of skin lesions confirmed the diagnosis of malignant syphilis, supported by serology results and he responded very well to doxycycline. It is important to recognize and diagnose malignant syphilis early and institute appropriate treatment as complete cure can be achieved. Keywords: Malignant syphilis, human immunodeficiency virus (HIV), MSM |
Introduction
The rate of primary and secondary syphilis reported in the United States is gradually increasing. Reported cases of syphilis decreased during the 1990s, were lowest in 2000, after which it gradually increased annually during 2001-20091. In a recent report published by CDC, primary and secondary syphilis rates have increased among men of all ages, races and ethnicities, largely among MSM, from 5.1 cases per 100,000 population in 2005 to 9.8 in 2013. Rates of 50%–70% HIV coinfection among MSM infected with primary and secondary syphilis have been reported2. Syphilis and the behaviours associated with acquiring it, increase the likelihood of acquiring and transmitting HIV. Although the incidence of HIV has remained stable, the incidence of syphilis has been increasing disproportionately possibly due to adaptive behaviour like serosorting among HIV concordant couples and oral sex that decrease transmission of HIV but not syphilis3.
Syphilis may manifest differently in patients with HIV. HIV positive patients present more often with secondary syphilis and the disease course is more aggressive4. Malignant syphilis also known as lues maligna or ulceronodular syphilis is a severe form of secondary syphilis and is more common among HIV infected persons5. Although HIV patients present with varied clinical symptoms, it is uncommon to present with florid secondary syphilitic skin lesions. Here we present a case report of a patient, who presented with diffuse ulceronodular skin lesions, whose serology and skin biopsy confirmed syphilis and was subsequently found to have HIV.
Case report
A 20-year-old African American man was admitted to Interfaith Medical Center with a generalised body rash for a month. He noticed a rash on his chest, which in few days spread centrifugally to his whole body, face and arms, including palms and soles. The rash was non-pruritic, painless, progressive in size and gradually oozed and crusted (Figure 1a). Besides significant unintentional weight loss of 26 pounds in the last two months, he did not report any other systemic complaints. He denied any travel or unwell contacts. He is a homosexual man and has had two male sexual partners in the last two years; one of them was treated for syphilis two years ago. He denied smoking, alcohol or drug use.

Figure 1a - Skin lesions reveal papulosquamous nodular and ulcerative changes in upper limbs
On admission, he was afebrile with normal vital signs. His physical examination revealed widespread papulonodular and ulcerated lesions on his whole body including the scalp and oral mucosa, and measured up to 2-3 cm. Skin lesions were prominent on his face, some with sero-purulent discharge and some covered with crusts and scabs, which would bleed on removal of crusts and scabs. No skin lesions were noted in genital area. Besides bilateral enlarged axillary lymph nodes, nosignificant lymphadenopathy was noted. Other systemic examinations were within normal limits.
His full blood count showed microcytic hypochromic anaemia with a mean corpuscular volume of 77.2 fL (normal reference range, 80-100 fL) and thrombocytosis with platelets of 546 per microliter (reference range, 130-400 per microliter). Renal and hepatic function tests were normal. He tested positive for HIV using serum enzyme linked immunosorbent assay (ELISA), rapid plasma reagin was 1:128 (reference range, nonreactive), fluorescent treponemal antibody absorption test was reactive (reference range, nonreactive) and neurosyphilis was ruled out with negative spinal fluid studies. Hepatitis B and Cserologieswere negative. Nucleic acid amplification test of the urine sample was negative for Neisseria gonorrhea and Chlamydia trachomatis. The patient was treated with doxycycline100 mg every 12 hours for secondary syphilis as he was allergic to penicillin.
The patient developed chills, fever, sweating, tachycardia and hypotension 18 hours after treatment with doxycycline. A Jarisch-Herxheimer reaction was suspected, which was managed with observation, intravenous hydration and a single dose of methylprednisone. Despite being on antibiotics, he had intermittent fever for two weeks, possibly related to the syphilis and its treatment. Further investigations included blood and urine culture, chest x-ray, CT scan of the head, chest, abdomen and pelvis and a gallium scan, which were unremarkable. Brucella IgM antibody, Q fever phase I and II antibodies, coccidioides antibody, histoplasma urine antigen, cryptococcal antigen and blood culture for acid fast bacilliwere all negative. His EBVserologies suggested past infection and CMV serologies for IgG and IgM were positive. Wound culture taken from the purulent skin lesions grew methicillin sensitive Staphylococcus aureus (MSSA)which was treated with antibiotics. His HIV-1 RNA was 1050118 (reference range, <20) and CD4 was 276 cells per microlitre (reference range, 317-1868 cells per microlitre), CD4 was 17.4% (reference range, 25.7-62.8%) and CD4:CD8 ratio was 0.32 (reference range, 0.20-3.50). Skin biopsy from the left forearm lesion showed lichenoid lymphohistiocytic infiltrate with plasma cells (Figure 1b). Immunochemical stain was positive for spirochetes, which confirmed secondary syphilitic skin lesions (Figure 1c). After three weeks of doxycycline therapy, significant clinical improvement in the skin lesions were noted. The skin lesions healed well with hyperpigmentation. Combination anti-retroviral therapy was initiated upon discharge and on follow-up a month later, the skin lesions had resolved and the RPR titre was 1:32; showing a four-fold reduction.
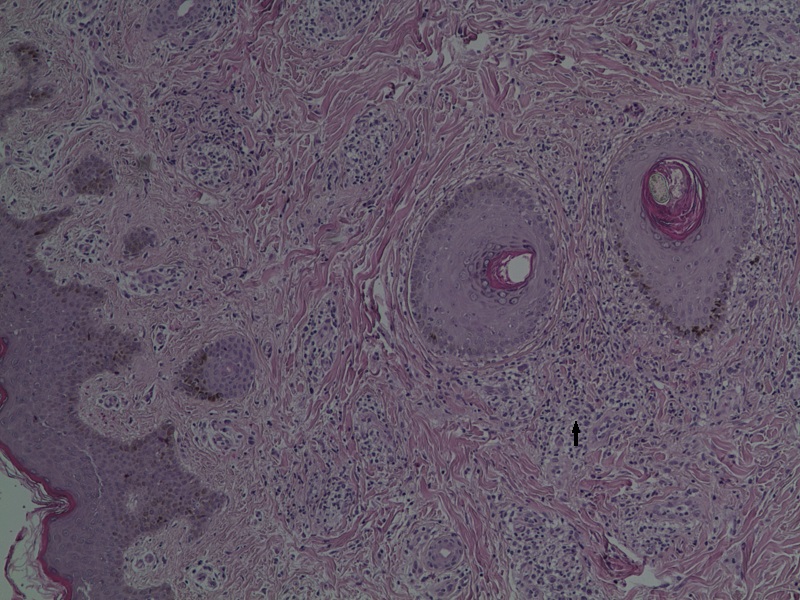
Figure 1b - A lymphocyhistiocytic infiltrate was present in the dermis and extended around blood vessels.
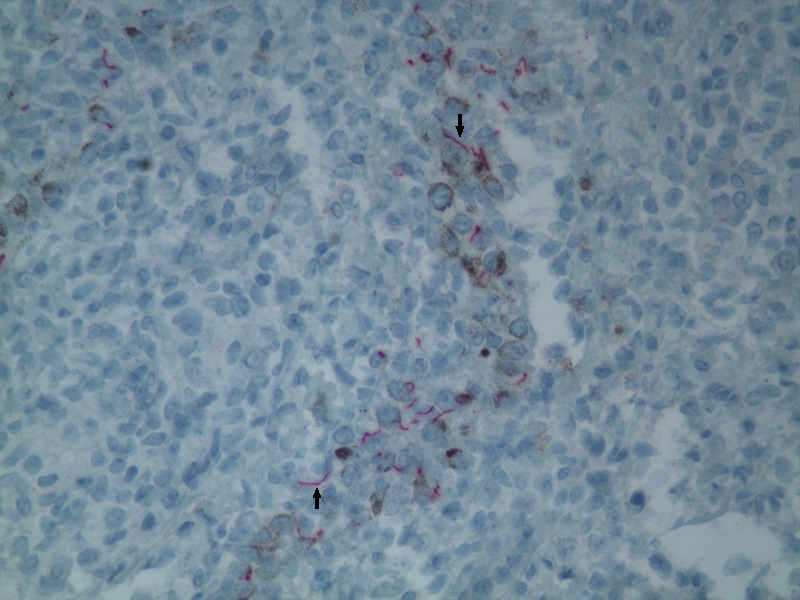
Figure 1c - Immunohistochemical stain showing delicate and spiral shaped spirochaetes, highly specific and sensitive of Treponema pallidum
Discussion
Skin lesions of secondary syphilis in patients with HIV may have varied appearance that mimic other diseases like cutaneous lymphomas, mycobacterial infections, bacillary angiomatosis, fungal infections or Kaposi’s sarcoma6. Detail workup was done in our patient and systemic fungal and bacterial infections were ruled out. He had secondary infection of the skin lesions due to MSSA and was treated with doxycycline. Skin biopsy confirmed secondary syphilitic skin lesions. Histology showed abundant plasma cells and lymphocytesandtreponomes were demonstrated in the special immuno-histochemical stains. Fisher’s diagnostic criteria for lues maligna include strongly positive RPR titre, a severe Jarisch-Herxheimer reaction, characteristic gross and microscopic morphology and rapid resolution of the lesions with antibiotics7. Our patient had all of these features. Because of variable presentation of skin lesions and increased rate of false negative serological tests due to prozone phenomenon in patients with HIV, alternative diagnostic techniques like biopsy of skin lesions and special stains should be performed8,9. The relative paucity of spirochetes in the biopsy of skin lesions makes the demonstration of microorganisms difficult. Yanagishawa et al were able to find 6 published cases of pathologically confirmed malignant syphilis with the demonstration of spirochetes10. Treatment of secondary syphilis in HIV infected patient is the same as that of HIV non infected patients. Benzathine penicillin is first line therapy and doxycycline is an alternative drug for penicillin allergic patients11. A severe Jarish-Herxheimer reaction occurred in our patient, which might not be observed in some cases with HIV and syphilis due to concurrent immunosuppression10. Experience from case reports have shown that malignant syphilitic skin lesions respond very well to antibiotics regardless of CD4 count12. With the increasing incidence of syphilis in HIV infected patients, it is important to recognise and diagnose malignant syphilis early and institute appropriate treatment as complete cure can be achieved.
|
Acknowledgements We acknowledge our pathologist Dr Shamah Iqbal, MD for providing the histopathology and immunostain photographs. Competing Interests None declared Author Details ASHOK R DEVAKOTA, MBBS, MD: Internal Medicine Resident, Interfaith Medical Center, Brooklyn, NY, USA. RABINDRA GHIMIRE, MBBS, MD: Infectious Disease Fellow, The Dr. James J. Rahal, Jr. Division of Infectious Diseases, New York Hospital Queens, NY, USA. MIRELA SAM, MD: Attending and Chief-Infectious Diseases, Interfaith Medical Center, Brooklyn, NY, USA. OO AUNG, MD: Internal Medicine Resident, Interfaith Medical Center, Brooklyn, NY, USA. CORRESPONDENCE: drrabindraghimire@gmail.com Email: drrabindraghimire@gmail.com |
References
- Division of STD prevention. Sexually Transmitted Disease Surveillance. C.D.C, 2012. Jan 2014:2.
- Patton, M.E., et al. Primary and secondary syphilis--United States, 2005-2013. MMWR Morb Mortal Wkly Rep, 2014;63(18):402-6.
- Mayer, K.H. and M.J. Mimiaga. Resurgent syphilis in the United States: urgent need to address an evolving epidemic. Ann Intern Med, 2011; 155(3):192-3.
- Lynn, W.A. and S. Lightman. Syphilis and HIV: a dangerous combination. Lancet Infect Dis, 2004;4(7):456-66.
- Zetola, N.M., et al. Syphilis in the United States: an update for clinicians with an emphasis on HIV coinfection. Mayo Clin Proc, 2007; 82(9):1091-102.
- Yayli, S., et al. Late secondary syphilis with nodular lesions mimicking Kaposi sarcoma in a patient with human immunodeficiency virus. Int J Dermatol, 2014;53(1): e71-3.
- Fisher, D.A., L.W. Chang, and D.L. Tuffanelli. Lues maligna. Presentation of a cas and a review of the literature. Arch Dermatol, 1969; 99(1):70-3.
- Pialoux, G., et al. Effect of HIV infection on the course of syphilis. AIDS Rev, 2008;10(2):85-92.
- Tucker, J.D., et al., Lues maligna in early HIV infection case report and review of the literature. Sex Transm Dis, 2009;36(8):512-4.
- Yanagisawa, N., et al. Pathologically confirmed malignant syphilis in an HIV-infected patient. Intern Med, 2011;50(20):2423-6.
- Zetola, N.M. and J.D. Klausner, Syphilis and HIV infection: an update. Clin Infect Dis, 2007;44(9):1222-8.
- Rallis, E. and V. Paparizos, Malignant syphilis as the first manifestation of HIV infection. Infect Dis Rep, 2012;4(1): e15.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




