Massive Hepatic Necrosis due to Hepatic Abscesses after Transplantation.
Seif Fadi, Gholam Pierre and Montenegro Hugo
Cite this article as: BJMP 2011;4(4):a439
|
|
Abstract Delayed hepatic artery thrombosis (HAT) is a rare complication of orthotopic liver transplantion (OLT) that may present with biliary sepsis or remain asymptomatic. Sonography is extremely sensitive for the detection of HAT in symptomatic patients during the immediate postoperative period. Magnetic resonance angiography (MRA) is a useful adjunct in patients with indeterminate ultrasound exams, those who have renal insufficiency or an allergy to iodinated contrast. In the absence of hepatic failure, conservative treatment appears to be effective for patients with HAT. Whole-graft orthotopic liver transplantation (OLT), Roux-en-Y biliary reconstruction, cold ischaemia and operative times, the use of blood and plasma, and the use of aortic conduits in arterial reconstruction are all risk factors associated with HAT. We present a patient with a case of delayed HAT three years after liver transplantation who presented with mild symptoms and was later found to have a massive hepatic abscess and significant necrosiswith positive cultures for Clostridium perfringens. There was evidence of complete occlusion of the hepatic artery 2 cm from its origin. |
Introduction:
The clinical features of early HAT are well defined, yet the features of delayed HAT are less clear. Delayed HAT is a rare complication of OLT that may present with biliary sepsis or remain asymptomatic. Sonography is extremely sensitive for the detection of HAT in symptomatic patients during the immediate postoperative period. However, the sensitivity of ultrasonography diminishes as the interval between transplantation and diagnosis of HAT increases due to collateral arterial flow. MRA is a useful adjunct in patients with indeterminate ultrasound exams and in those who have renal insufficiency or an allergy to iodinated contrast.
In the absence of hepatic failure, conservative treatment appears to be effective for patients with HAT but retransplantation may be necessary as a definitive treatment.
Case Presentation:
A 52 year old male with a history of whole graft OLT for primary sclerosing cholangitis presented with two days of fever, nausea, and mild abdominal discomfort.
One week prior to presentation, he was seen in the liver clinic for regular follow-up. At that time, he was totally asymptomatic and his laboratory workup including liver function tests were within normal range.
He has undergone OLT three years prior. At the time of transplant he required transfusion of 120 units of packed red blood cells, 60 units of fresh frozen plasma and 100 units of platelets due to extensive intraoperative bleeding secondary to chronic changes of pancreatitis and severe portal hypertension, but had an otherwise uneventful postoperative recovery.
On physical examination the temperature was 39C, heart rate was 125 beats per minute, respiratory rate was 22 bpm. Initial laboratory workup revealed a white blood cell count of 25,000/mm3, AST of 6230 U/L, ALT of 2450 U/L, total bilirubin of 11 mg/dL , BUN 55 mg/dL and Creatinine of 4.5 mg/dL. Lactate level was 5 mmol/L. Doppler ultrasonography revealed an extensive intrahepatic gas (Image 1A). Computed tomography of the abdomen and pelvis revealed extensive area of hepatic necrosis with abscess formation measuring 19x14 cm with extension of gas into the peripheral portal vein branches (Image 1B,C). Upon admission to the hospital, the patient required endotracheal intubation, mechanical ventilator support and aggressively fluid resuscitation. He was started on broad-spectrum antibiotics and a percutaneous drain was placed that drained dark, foul smelling fluid. Cultures from the blood and the drain grew Clostridium perfringens.
Magnetic resonance imaging (MRI), MRA revealed occlusion of the hepatic artery 2 cm from its origin and also evidence of collaterals (Image 2A,B).
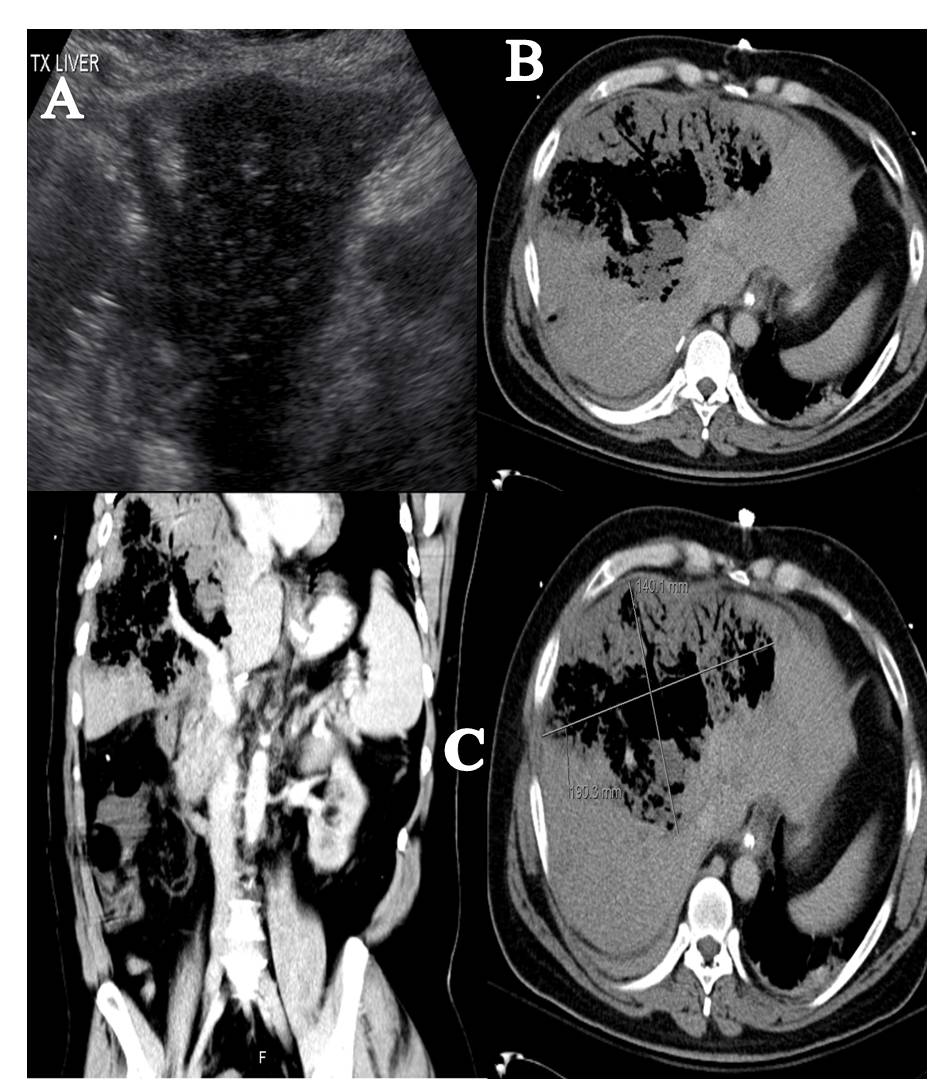
Image 1: (Pannel A) Doppler ultrasonography reveal extensive intrahepatic gas. (Pannel B&C) Computed tomography of the abdomen and pelvis reveal an extensive area of hepatic necrosis with abscess formation measuring 19x14 cm with extension of gas into the peripheral portal vein branches.
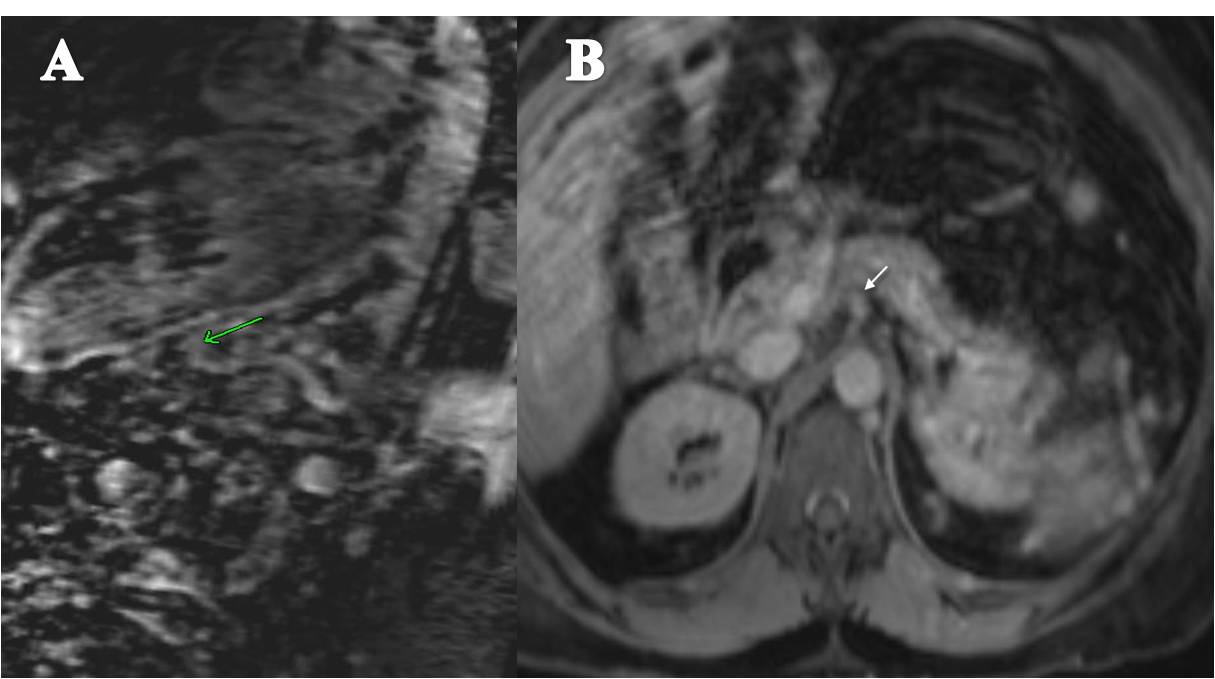
Image 2: MRI & MRA reveal occlusion of the hepatic artery 2 cm from its origin and also evidence of collaterals.
Following drain placement, the patient’s clinical condition markedly improved with significant reduction of liver function test values. Retransplantation was considered but delayed in the setting of infection and significant clinical and laboratory testing improvement.
The patient was transferred to the medical floor in stable condition, and the drain was then removed.
A week later the patient developed low grade fevers and tachycardia. One day later he began to experience mild abdominal discomfort and high grade fevers. Repeat CT of the abdomen revealed worsening hepatic necrosis and formation of new abscesses. His clinical condition decompensated quickly thereafter requiring endotracheal intubation, mechanical ventilation and aggressive resuscitation. Percutaneous drain was placed and again, drained pus-like, foul-smelling material. His overall condition deteriorated, and he eventually expired a few days later.
Discussion:
Delayed (more than 4 weeks after transplantation) HAT is a rare complication of OLT with an estimated incidence of at around 2.8%1.
Risk factors associated with development of HAT include Roux-en-Y biliary reconstruction, cold ischaemia and operative time, the use of greater than 6 units of blood, the use of greater than 15 units of plasma, and the use of aortic conduits on arterial reconstruction during transplant surgery2.
Collateralization is more likely to develop after Live Donor Liver Transplantation (LDLT) than after whole-graft cadaveric OLT3. Therefore, the latter is also associated with increased risk of late HAT.
Although the clinical features of early HAT are well described, the features of delayed HAT are less clearly defined1: the patient may present with manifestations of biliary sepsis or may remain asymptomatic for years. Right upper quadrant pain has been reported to occur in both immediate and delayed HAT. The clinical presentations may include recurrent episodes of cholangitis, cholangitis with a stricture, cholangitis and intrahepatic abscesses, and bile leaks1. Doppler ultrasonography has been extremely sensitive for the detection of HAT in symptomatic patients during the immediate postoperative period but becomes less sensitive as the interval between transplantation and diagnosis of HAT increases because of collateral arterial flow4.
3D gadolinium-enhanced MRA provides excellent visualization of arterial and venous anatomy with a fairly high technical success rate. MRA is a useful adjunct in patients with indeterminate ultrasonography examination in patients who have renal insufficiency or who have allergy to iodinated contrast 5.
Antiplatelet prophylaxis can effectively reduce the incidence of late HAT after liver transplantation, particularly in those patients at risk for this complication6. Vivarelli et al reported an overall incidence of late HAT of 1.67%, with a median time of presentation of 500 days; late HAT was reported in 0.4% of patients who were maintained on antiplatelet prophylaxis compared to 2.2% in those who did not receive prophylaxis6. The option of performing thrombolysis remains controversial. Whether thrombolysis is a definitive therapy or mainly a necessary step in the proper diagnosis of the exact etiology of HAT depends mostly on the particular liver center and needs further analysis7. Definitive endoluminal success cannot be achieved without resolving associated and possible instigating underlying arterial anatomical defects. Reestablishing flow to the graft can unmask underlying lesions as well as assess surrounding vasculature thus providing anatomical information for a more elective, better plan and definitive surgical revision7. Whether surgical revascularization compared to retransplantation is a viable option or only a bridging measure to delay the second transplantation has been a longstanding controversy in the treatment of HAT.
Biliary or vascular reconstruction do not increase graft survival and ongoing severe sepsis at the time of re-graft results in poor survival7. However, although uncommon, delayed HAT is a major indication for re-transplantation7. In the absence of hepatic failure, conservative treatment appears to be effective for patients with hepatic artery thrombosis.
C. perfringensis an anaerobic, gram-positive rod frequently isolated from the biliary tree and gastrointestinal tract. Inoculation of Clostridium spores into necrotic tissue is associated with formation of hepatic abscess8.
Necrotizing infections of the transplanted liver are rare. There have been around 20 cases of gas gangrene or necrotizing infections of the liver reported in the literature. Around 60% of these infections were caused by clostridial species with C. perfringens accounting for most of them. Around 80% of patients infected with Clostridium died, frequently within hours of becoming ill9,10. Those who survived underwent prompt retransplantation and the infection had not resulted in shock or other systemic changes that significantly decreased the likelihood of successful retransplantation8.
Because the liver has contact with the gastrointestinal tract via the portal venous system, intestinal tract bacteria may enter the liver via translocation across the intestinal mucosa into the portal venous system. Clostridial species can also be found in the bile of healthy individuals undergoing cholecystectomy9,10.
The donor liver can also be the source of bacteria. Donors may have conditions that favor the growth of bacteria in bile or the translocation of bacteria into the portal venous blood. These conditions include trauma to the gastrointestinal tract, prolonged intensive care unit admissions, periods of hypotension, use of inotropic agents, and other conditions that increase the risk of potential infection 8,9,10. C. perfringens sepsis in OLT recipients has been uniformly fatal without emergent retransplantation. Survival from C. perfringens sepsis managed without exploratory laparotomy or emergency treatment has been extremely rarely reported8. In those patients who survived, and in whom the infection has not resulted in shock or multiple organ failure, retransplantation may be successful8.
Although our patient survived his intensive care course, his recovery was tenuous as he quickly developed additional hepatic abscesses that led to his eventual demise. Post-mortem examination in our patient revealed intra-hepatic presence of Clostridium perfringens.
He was managed conservatively since he markedly improved both clinically and by liver function tests. Because of this, retransplantation was delayed. He was also already on antiplatelet prophylaxis.
Conclusion:
We report an interesting case of Clostridium perfringens hepatic abscess due to late HAT following OLT. Although the patient initially improved with non-surgical treatment, he eventually died. In similar cases, besides aggressive work-up and medical management retransplantation may be necessary for a better long term outcome.
|
Competing Interests None declared Author Details SEIF FADI, M.D. Fellow, Pulmonary Critical Care and Sleep Medicine, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine. GHOLAM PIERRE, MD. Associate Professor of Medicine Medical Director, Hepatology. Division of Gastroenterology and Liver Disease, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine. MONTENEGRO HUGO, M.D. Professor, Pulmonary Critical Care and Sleep Medicine, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine. Louis Stokes Cleveland VA Medical Center. CORRESPONDENCE: MONTENEGRO HUGO, University Hospitals Case Medical Center, Case Western Reserve, Case Western Reserve University School of Medicine. Louis Stokes Cleveland VA Medical Center. Email: Hugo.Montenegro@UHhospitals.org |
References
1. Bhattacharjya S, Gunson BK, Mirza DF, et al. Delayed hepatic artery thrombosis in adult orthotopic liver transplantation-a 12-year experience. Transplantation 2001; 71(11):1592-6.
2. Silva M, Jambulingam P, Gunson B, et al. Hepatic artery thrombosis following orthotopic liver transplantation: A 10-year experience from a single centre in the United Kingdom. Liver Transplantation 2006; 12:146-151.
3. Tian MG, Tso WK, Lo CM et al. Treatment of hepatic artery
thrombosis after orthotopic liver transplantation. Asian J Surg. 2004; 27(3):213-7.
4. Horrow M, Blumenthal B, Reich D et al. Sonographic Diagnosis and Outcome of Hepatic Artery Thrombosis After Orthotopic Liver Transplantation in Adults. AJR 2007; 189:346-351.
5. Ishigami K, Stolpen A, Al-kass F et al. Diagnostic Value of Gadolinium-Enhanced 3D Magnetic Resonance Angiography in Patients With Suspected Hepatic Arterial Complications After Liver Transplantation. Journal of Computer Assisted Tomography 2005; 29(4):464-471.
6. Vivarelli M, La Barba G, Cucchetti A, et al. Can antiplatelet prophylaxis reduce
the incidence of hepatic artery thrombosis after liver transplantation? Liver
Transpl 2007; 13:651-654.
7. Perkins J. Thrombolysis for early hepatic artery thrombosis: Definitive
therapy or diagnostic aid? Liver Transplantation 2007; 13:927– 931.
8. Diaz G, Boyer T, Renz J. Survival of Clostridium perfringens. Sepsis in a Liver Transplant Recipient. Liver Transplantation 2009; 15:1469-1472.
9. Doblecki-Lewis S, Palaios E, Bejarano PA et al. Hepatic gas gangrene following orthotopic liver transplantation: three cases treated with re-transplantation and a review of the literature. Transpl Infect Dis.2008; 10:280–285.
10. Eigneberger B, Königsrainer I, Kendziorra H et al. Fulminant liver failure due to Clostridium perfringens sepsis 9 years after liver transplantation. Transpl Int.2006; 19:172–173.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




