An overview of prolonged disorders of consciousness for the General Practitioner
Adam Boardman & Ganesh Bavikatte
Cite this article as: BJMP 2020;13(1):a007
|
|
Abstract The incidence of hospital admissions due to acquired brain injury is increasing, and due to increased survival rates there are a higher proportion of patients are discharged with complex disabilities including prolonged disorders of consciousness. These patients are largely cared for in the community by General Practitioners, with occasional input from specialist teams. This article combines latest guidance from the British Medical Association and Royal College of Physcians with our own experience as Rehabilitation Medicine physicians, with the aim of improving confidence in managing patients with vegetative state and minimally conscious state, and increasing understanding of the associated medicolegal and ethical issues. Keywords: Prolonged disorders of consciousness; Vegetative state; Minimally conscious stateAbbreviations: ABI: acquired brain injury; PDOC: prolonged disorders of consciousness; MCS: minimally conscious state; VS: vegetative state; GP: General Practitioner ; RCP: Royal College of Physicians; BMA: British Medical Association; EEG: electroencephalography; WHIM: Wessex Head Injury Matrix; CRS-R: JFK Coma Recovery Scale-Revised; SMART: Sensory Modality Assessment and Rehabilitation Technique; CPR: cardiopulmonary resuscitation; MDT: multidisciplinary team; CANH: clinically assisted nutrition and hydration; COP: Court of Protection |
Introduction
Since 2005, there has been an increase of 10% in hospital admissions with acquired brain injury (ABI), with 348,453 United Kingdom (UK) admissions in 2016-17.1 With improvements to both medical and surgical management, a higher proportion of patients survive to hospital discharge, resulting in more people with complex physical and cognitive disabilities reaching the community.2,3
Prolonged disorders of consciousness (PDOC) can occur following ABI. This can vary from coma, to vegetative state (VS), and minimally conscious state (MCS). Following acute stabilisation, the treating team must provide the correct diagnosis, prognosis, and management. Ethical and legal issues, such as best interests decision-making (considering patient wishes, advanced decisions, and best possible quality of life), deciding when appropriate to provide end-of-life care, and understanding the legal framework around these issues can further complicate the process.
Whilst there is currently no national registry for patients with PDOC, information taken from patients in nursing homes in the UK give an estimated 4000 – 16000 patients in VS, and up to three times this many in MCS.4
Early and ongoing assessment of the patient is vital, as is good communication with those close to the patient, and an understanding of the legal requirements of the treating clinician. These are likely to present even more of a challenge to General Practitioners (GP) in the community who are managing these patients as part of their larger responsibilities.
This review article summarises guidance from the Royal College of Physicians (RCP) and British Medical Association (BMA), in conjunction with our own clinical experience, to improve understanding surrounding the assessment, long term management, and the ethical and legal issues in patients with PDOC, aiming to improve the confidence of clinicians managing these patients.5,6
Identifying Patients
Consciousness requires a combination of wakefulness and awareness (self and environment). Patients with significant deficits in either of these can be said to have a disorder of consciousness. Various brain injuries can result in disorders of consciousness (see Table 1).
Table 1: Aetiology of acquired brain injury.5
| Cause | Examples |
| Vascular | Stroke, subarachnoid haemorrhage |
| Hypoxic | Cardiac arrest, hypovolaemia |
| Infection / inflammatory | Encephalitis, vasculitis |
| Trauma | Primary brain trauma, diffuse axonal injury |
| Metabolic / Endocrine | Hypoglycaemia, drug overdose, alcohol |
| Degenerative | Primary neurodegenerative conditions such as dementia |
This article focuses on acute causes of PDOC rather than those with primary neurodegenerative conditions, as they present separate clinical entities with different issues affecting prognosis and management choices.
Disorders of consciousness, like a sliding scale, vary from coma, to VS, and MCS:
- Coma - unrousable unresponsiveness. Patients cannot be roused, lack a sleep-wake cycle, exhibit no purposeful movement, and do not respond to stimuli.
- VS - wakefulness but not awareness. Patients have a sleep-wake cycle and open their eyes spontaneously, but lack awareness of self or their environment. These patients can exhibit spontaneous and reflexive movements, and external stimuli can produce arousal responses.
- MCS - wakefulness but reduced or inconsistent awareness. Patients have a sleep-wake cycle and demonstrate reproducible but inconsistent awareness of self, and ability to interact with others and their environment.
Diagnosis
As per RCP guidance 2020, patients with impaired consciousness for over 4 weeks are deemed to have PDOC.5 It is first important to differentiate possible VS / MCS from other conditions:5
- Abnormalities on electroencephalography (EEG) can aid diagnosis of coma. These patients tend to progress to VS or death within weeks, so assessments of consciousness are not appropriate during this period.
- Patients with locked-in syndrome have wakefulness and awareness, but paralysis of the limbs and majority of facial musculature, preventing communication by these means. EEG in locked-in syndrome is usually normal, and patients may be able to communicate using eye movements.
- Patients with brainstem death have loss of all brainstem reflexes and respiratory effort, and organ survival is only temporarily achieved with life support machines.
Once ‘mimic’ conditions are ruled out, making a diagnosis of VS or MCS in patients with a suspected disorder of consciousness follows a 3-step process with input of clinicians trained in the management of PDOC:
1. Establishing a cause
This can be straightforward in some cases, such as those with direct trauma to the brain, or acquired brain infections or inflammation causing structural damage to the brain. In other cases this can be more difficult, and it may not possible to reach an exact diagnosis. The treating clinician must establish that the patient’s current condition is due to a brain injury, and take reasonable steps to determine the cause.
2. Reversible causes should be excluded
This includes reviewing medications to stop sedative medications whenever possible, blood tests to look for infection or metabolic / electrolyte abnormalities, up-to-date imaging to rule out new onset hydrocephalus, or performing an EEG to rule out subclinical seizures needing antiepileptic medication. This step also includes establishing that neurological pathways are intact, so that any assessment of consciousness provides an accurate reflection of the patient’s condition. Briefly, this involves examination and investigations to confirm that sensory, visual, auditory, and motor pathways are intact.
3. Structured assessment
There are several tools available which can confirm the diagnosis of VS or MCS. All of these require a trained assessor and an appropriate environment. These tools provide a structured method of assessing the patient to:
- Observe spontaneous behaviours.
- Observe the patient’s reaction to stimuli from different sensory modalities.
- Document the findings of family / friends / members of the healthcare team following their interactions with the patient.
Tools available include the Wessex Head Injury Matrix (WHIM), the JFK Coma Recovery Scale-Revised (CRS-R), and the Sensory Modality Assessment and Rehabilitation Technique (SMART), amongst others. As per RCP guidance, the CRS-R should be the primary assessment tool, and WHIM or SMART can be used to provide additional information. Furthermore, assessments need to be performed on at least 10 occasions, at several different times of the day, and over the course of a 2-3 week period.5,7-9
The 2020 RCP guidance also addresses how to manage patients that do not present through the acute hospital pathway.5 In these ‘late assessment’ cases, formal assessment is still required to establish their level of consciousness and guide management. These patients should be referred to an experienced PDOC assessor to establish the cause of PDOC, rule out reversible causes, and arrange formal evaluation. This should ideally be achieved by outreach assessments, but if this is not possible, structured interviews should be held with family and care staff to complete the CRS-R. If these measures do not provide a definite diagnosis, admission to a PDOC centre can be considered.5,8
Vegetative State & Minimally Conscious State
Patients in VS are unable to interact with their surroundings or those around them (no voluntary behaviours / communication / purposeful movements), and show no evidence of awareness of self. The patient may demonstrate reflexive behaviour (such as increased heart rate or startle response to noise), or spontaneous, purposeless movements (such as eye movements, teeth grinding, or limb movements). These behaviours can be misleading, which is why an objective and structured assessment method is vital.
Patients in MCS have some evidence of awareness of self or their environment, on a reproducible but inconsistent basis. Patients demonstrate behaviours such as: following simple commands, verbalisation, and purposeful behaviour MCS which is further classified based on the level of responsiveness:
- MCS-minus - less complex behaviours such as orientation to noxious stimuli, or purposeful eye movements.
- MCS-plus - more complex behaviours such as following instructions or interacting with objects.
Prognosis depends on cause, time since brain injury, and the trajectory of improvement (better prognosis for those who quickly progressed from VS to MCS). Those with traumatic brain injury are more likely to regain awareness and have a longer window for potential recovery. The majority of VS patients that regain consciousness tend do so within 12 months in traumatic cases, and 3 months in non-traumatic cases. The majority of MCS patients that regain consciousness do so within 2 years post injury, although others can emerge at up to 4 years. Whilst these are the expected outcomes, there are, however, rare case reports of patients emerging later than this.
VS / MCS-minus are classed as ‘continuing’ at >4 weeks post brain injury, and ‘chronic’ at >3 months for non-traumatic cases, or >12 months in traumatic cases. MCS-plus is classed as ‘continuing’ at >4 weeks post brain injury, and ‘chronic’ at >9 months for non-traumatic cases, or >18 months in traumatic cases. Chronic VS / MCS can be classed as ‘permanent’ when there has been no further change in trajectory of serial CRS-R for 6 months. In permanent PDOC it is predicted that consciousness is highly improbable to recover. It is important to remember these time frames, and their implications during discussions with family, when making best interests decisions and planning further assessments of consciousness.5,10,11
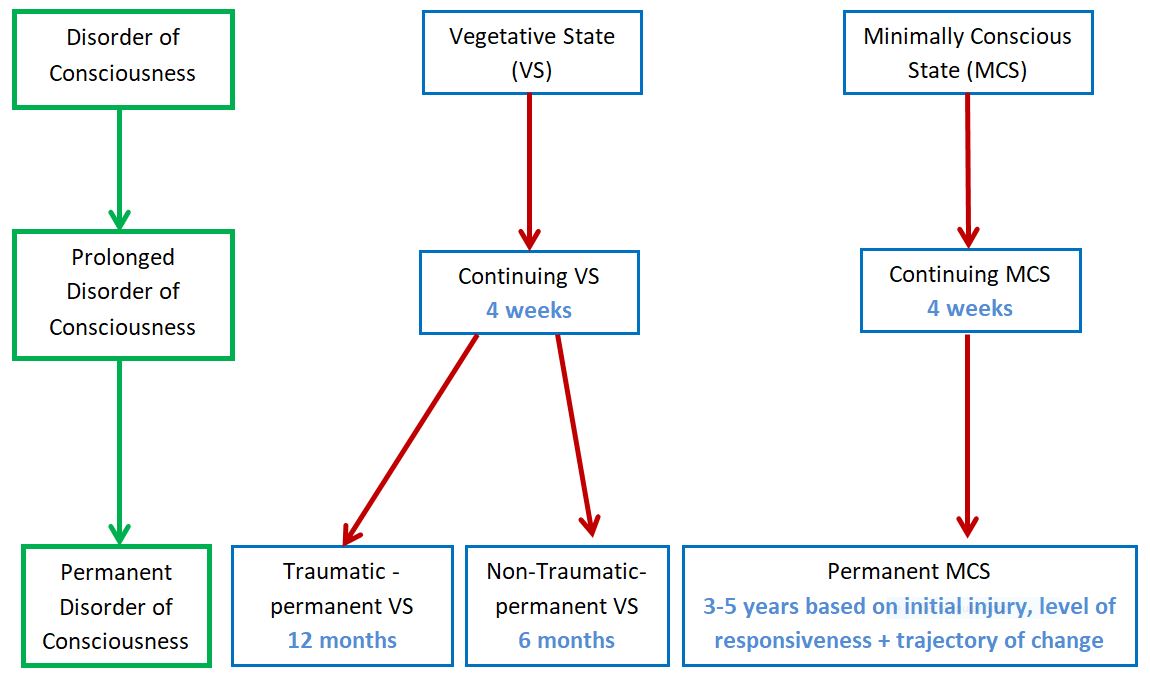
With the longer time period for potential emergence, and improved survival rate compared to VS, GPs are more likely to come across these patients in the community. Figure 1 outlines the key time points for assessment of VS and MCS.12
Figure 1: Timeline for assessment of VS & MCS.5
Emergence
A patient is considered to have ‘emerged’ from PDOC if they are able to consistently demonstrate awareness of self and surroundings. The RCP advise that patients who have emerged are able to do at least one of the following:5
- Functional interactive communication (accurate yes/no responses to 6/6 basic questions on 2 consecutive evaluations).
- Functional use of objects (intelligent use of ≥2 objects on 2 consecutive evaluations).
- Consistent discriminatory choice-making (correct identification between 2 pictures, 6/6 times, on 2 consecutive evaluations).
Specialist Involvement
Early specialist input from a neurological rehabilitation team is recommended. The Royal College of Physicians Guideline Development Group advise that those with an ongoing disorder of consciousness at 4 days (Glasgow Coma Scale ≤10/15) should be referred for assessment, and advice regarding neurological disability and prevention of complications.5,13 At 2 weeks the patient should be referred for specialist neurological evaluation to identify the cause of the disorder of consciousness, assess the primary neurological pathways, and advise on further investigations.
Patients with ongoing disorder of consciousness at 4 weeks should have regular input from a specialist neurological rehabilitation team, led by a consultant in Rehabilitation Medicine. Once stable the patient should ideally be transferred to a specialist neurorehabilitation unit for multidisciplinary care, objective assessment of level of consciousness, formal best interests decision-making, and discharge planning.
Following this initial period, the patient should be placed in a unit away from the acute setting, where they can be monitored until it is evident that they are likely to remain in VS / MCS. These ‘slow-stream’ rehabilitation units, are designed to deliver care to patients with complex neurological disability, and provide appropriate maintenance therapy to manage physical disability. Medical input is usually provided by the GP surgery covering the area, although units should also have access to rehabilitation medicine physicians with experience in managing PDOC.
If it is agreed that a patient has permanent VS / MCS, then longer-term of care can be provided in a nursing home or, if appropriate, in the patient’s own home. A skilled assessor should review the patient yearly, with formal assessment of consciousness until either the patient emerges or dies.
Medicolegal & Ethical Issues
Capacity Assessments
By definition a person in PDOC lacks capacity to make decisions about medical treatment. The Mental Capacity Act 2005 requires this to be formally documented in the medical notes. A Deprivation of Liberty Safeguard should be put in place during hospital admission or nursing / residential home stay, providing that restraint and restrictions are in the patient’s best interests.14
Identifying Advance Decisions
The team providing care need to identify as early as possible whether the patient has a valid and relevant Advance Decision, Health and Welfare Lasting Power of Attorney, or Court-appointed Welfare Deputy. If one of these is in place, the team need to request to see the relevant documentation to understand what exactly it entails.
Best Interests Meetings
All medical treatment provided must be in the patient’s best interests. In the UK, the treating clinician must by law identify those people close to the patient that can provide insight into the patient’s beliefs / previous expressed wishes / likely wishes, and take part in best interests meetings. If there is nobody to fulfil this role then an Independent Mental Capacity Advocate must be appointed. An initial best interests meeting should be held to discuss the diagnosis, likely prognosis, and to plan treatment. Further meetings should be held at planned regular intervals, for major medical decisions, and following repeat assessments to decide future management, discharge planning, and ceilings of care.
Ceiling of Care Discussions:
Many relatives may not feel comfortable bringing up these topics themselves, so it is advisable to make the discussion part of a routine review as standard for PDOC patients.
In patients with PDOC, cardiopulmonary resuscitation (CPR) has a very low success rate, and will likely result in further brain injury due to hypoxia. For the majority of patients where emergence is not expected, or if it is felt that the patient would not accept their level of quality of life, CPR could be considered to be futile. This is because CPR would not provide a perceivable benefit to the patient, but would carry significant risks of harm (worsening brain injury, injury related to the CPR itself, undignified end of life). Decisions regarding ceiling of care or appropriateness of resuscitation should either follow the instructions set out in existing advanced directives, or be discussed together with the treating multidisciplinary team (MDT). It is highly advisable to involve close family / friends in discussions, but ultimately it is a medical decision.
For similar reasons, it should be considered whether hospital admission for treatment of acute deterioration is in the patient’s best interests. For example in a patient with permanent VS, treating an acute chest infection may improve their lungs, but will not improve the patient as a whole in a way that can be perceived and appreciated by that patient, so may be considered futile. Additionally, it may be considered appropriate to stop medications not aimed at providing comfort, or stop performing observations and investigations. As with all major medical decisions, this should be discussed within the MDT and with those close to the patient. Although patients with PDOC have absent / reduced awareness, care should be taken to maximise patient comfort, and if appropriate consider input from the palliative care team.
Decisions relating to withdrawing clinically assisted nutrition and hydration (CANH) have previously been managed differently than withdrawal of life-sustaining treatment. Until recently, the decision to withdraw CANH could not be made without referring to the Court of Protection (COP). More recent guidance published by the BMA advises that in PDOC this is not always necessary. The treating team should first establish whether there are any valid and relevant advance directives / health and welfare attorney with relevant power, and then follow a best interests decision-making process. If all parties are agreed that withdrawal of CANH is in the patient’s best interests, then a second opinion should be obtained (from an independent, expert PDOC physician); if they also agree, then CANH can be withdrawn. If there is any doubt or disagreement about the decision, then an application to the COP is required. Now in the UK, it is essential to have best interests meetings to decide whether provision or continuation of CANH is of benefit to the patient, rather than deciding whether to withdraw it. If CANH is determined to not be of overall benefit to the patient, then it should not be continued. Prior to the withdrawal of CANH, an appropriate end-of-life care plan should be agreed and be ready to put in place.6
Conclusion
Disorders of consciousness can occur following brain injury, and vary from coma to MCS. If the disorder of consciousness continues for 4 weeks, it is described as a PDOC. Diagnosis requires structured assessment by trained clinicians, once the patient is medically optimised and reversible causes are excluded. Ongoing assessment is crucial to monitor recovery, guide prognosis, and establish when the disorder is permanent.
There are many ethical and medicolegal issues involved in managing patients with PDOC, which are mainly centred on the patient’s loss of mental capacity to make decisions. The cost implications of providing care as outlined in these guidelines can be quite significant. This article reflects our experience working within the National Health Service (NHS) within the UK, which provides free healthcare to all at the point of delivery. Therefore the costing is less relevant to the patients, although this does need to be considered when commissioning services. In other private healthcare settings, costs may vary widely based on hospital and wider multidisciplinary team costs, and this may need to be taken into account when commissioning services. Also, we appreciate that in other countries there are likely to be different laws surrounding PDOC, and varying views regarding the ethical decisions discussed.
Currently, these guidelines are based on expert opinion from the Royal College of Physicians Guideline Development Group. In future, management of patients with PDOC could be improved with the establishment of a national registry, further studies into PDOC, and better integration with community services. Furthermore, an improved education about PDOC and the issues surrounding it, as we have aimed to outline in this article, will help physicians understand their responsibilities and provide the best possible patient care.
|
Competing Interests None declared Author Details ADAM BOARDMAN, MBChB, MRCP UK, Complex Rehabilitation Unit, Sid Watkins Building, The Walton Centre Foundation Trust, Lower Lane, Liverpool, L9 7BB, United Kingdom. GANESH BAVIKATTE, MBBS, MD (Medicine), FRCP (London), FEPRM (Europe), Complex Rehabilitation Unit, Sid Watkins Building, The Walton Centre Foundation Trust, Lower Lane, Liverpool, L9 7BB, United Kingdom. CORRESPONDENCE: Adam Boardman, Complex Rehabilitation Unit, Sid Watkins Building, The Walton Centre Foundation Trust, Lower Lane, Liverpool, L9 7BB, United Kingdom. Email: adam.boardman1@nhs.net |
References
- Headway. Acquired brain injury 2016-2017 statistics based on UK admissions. 2018. https://www.headway.org.uk/about-brain-injury/further-information/statistics/, (accessed 29 July 2019).
- Caplan H, Cox C. Resuscitation Strategies for Traumatic Brain Injury. Current Surgery Reports Epub 2019 May 15. 7. 10.1007/s40137-019-0237-x.
- Stroke Association. State of the nation: Stroke statistics. February 2018. Available online at {https://www.stroke.org.uk/system/files/sotn_2018.pdf}.
- Vegetative and Minimally Conscious States. Houses of Parliament POSTNOTE. PN489, 2015.
- Prolonged disorders of consciousness following sudden onset brain injury: National clinical guidelines. London: Royal College of Physicians, 2020.
- British Medical Association. Clinically-assisted nutrition and hydration (CANH) and adults who lack the capacity to consent: Guidance for decision-making in England and Wales. 2019.
- Shiel A, Horn SA, Wilson BA, et al. The Wessex Head Injury Matrix (WHIM) main scale: a preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin Rehabil 2000; 14:408-16.
- Giacino, J & Kalmar, K. (2006). Coma Recovery Scale-Revised. The Center for Outcome Measurement in Brain Injury.
- Gill-Thwaites H, Munday R. The Sensory Modality Assessment and Rehabilitation Technique (SMART): A valid and reliable assessment for vegetative state and minimally conscious state patients. Brain Inj 2004;18(12):1255-1269.
- Luaute J, Maucort-Boulch D, Tell L et al. Long-term outcomes of chronic minimally conscious and vegetative states. Neurology 2010;75:246–52.
- Katz DI, Polyak M, Coughlan D et al. Natural history of recovery from brain injury after prolonged disorders of consciousness: outcome of patients admitted to inpatient rehabilitation with 1–4 year follow-up. Prog Brain Res 2009;177:73–88.
- Faugeras F, Rohaut B, Valente M, Sitt J, Demeret S, Bolgert F., et al. Survival and consciousness recovery are better in the minimally conscious state than in the vegetative state. Brain Injury 2018; 72–7.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13;2(7872):81-4.
- Mental Capacity Act 2005. London: HMSO.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




