Pneumocephalus after Epidural Anesthesia
Murtaza Rashid, Mohammad Al Mogbil, Bader Al Otaibi & Majid Al Johani
Cite this article as: BJMP 2018;11(2):a1113
|
|
Abstract We present case report of a patient who developed Pneumocephalus after epidural anaesthesia for labor pain. A 39 year old female presented to our Emergency Department with severe headache. Few days prior she had normal vaginal delivery aided by epidural anaesthesia. Brain CT scan showed Pneumocephalus which was treated conservatively. Epidural anaesthesia is commonly used in patients having labor pain. It is one of the safe procedures if performed by expert hands and with proper equipment. One of the very uncommon complication and rarely reported is Pneumocephalus which should alert a physician in case of persistent headache following the procedure. Keywords: Pneumocephalus, Epidural Anesthesia |
Introduction
Epidural anaesthesia is one of the favored and effective treatment options for labour pain. It is usually safe and only a handful situations lead to absolute contraindications to this technique such as patient’s refusal, lack of expertise and equipment, severe coagulopathy and infection at the site of puncture (1). However, as with any other technique and procedure, epidural anaesthesia is not flawless. The side effects and complications include hypotension, pruritus, inadequate analgesia, post puncture headache, nerve damage, infection, and epidural haematoma (1,2). Headache is common in one third of the patients after lumbar puncture however, the frequency is less in epidural anaesthesia as the fluid is injected in and not removed in the latter (3). Accidental dural damage and subsequent headache following epidural anaesthesia is uncommon and is an important cause of morbidity which can limit patient severely. Further, in rarest of rare cases Pneumocephalus can develop after epidural anaesthesia which has rarely been reported. We report a patient who developed Pneumocephalus after receiving epidural anaesthesia for labour pain.
Case Report:
A 39 year old female presented to our Emergency Department with severe headache not responsive to analgesics. The headache started developing 10 to 12 hours after she was given an epidural which was attempted three times for labour pain which was four days prior at a nearby medical center . The severity of the headache did not change with lying or the upright position. She had no symptoms of vomiting, no fever and no confusion. Neurological examination and vital signs were unremarkable. The site of the spinal anaesthesia did not reveal any swelling or any signs of infection. An urgent head CT scan was performed which revealed Pneumocephalus denoted by numerous left fronto-parietal extra axial air locules (Figure 1 and Figure 2). MRI spine revealed mild subcutaneous oedema at the site of the needle insertion without any haemorrhage or collection. The patient was admitted and treated conservatively for six days and follow up serial head CT scans showed complete resorption of the Pneumocephalus and the patient’s symptoms resolved completely. The patient was discharged and the follow up was uneventful.
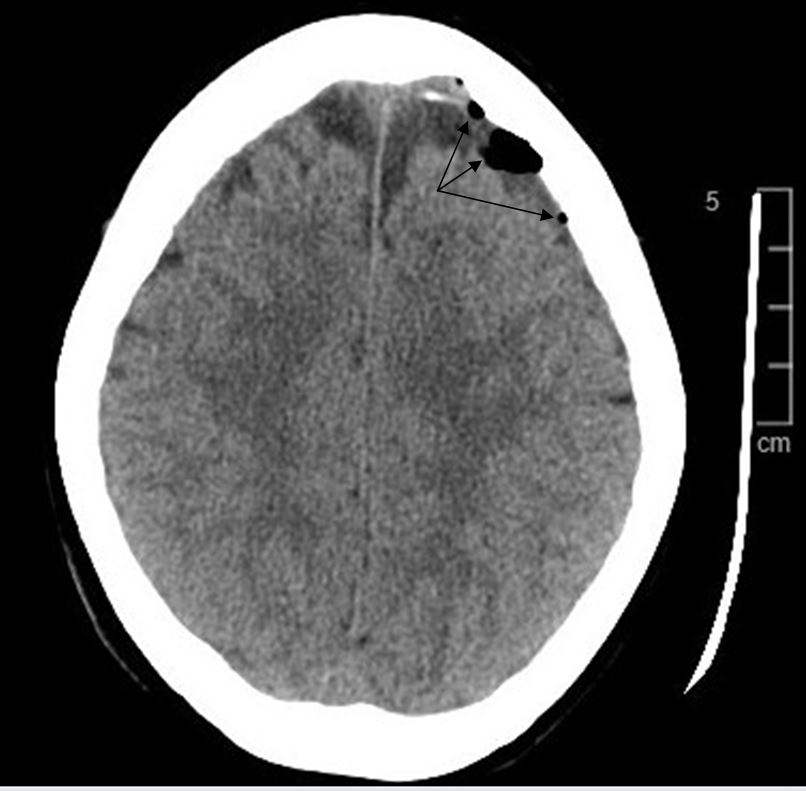
Figure 1: Pneumocephalus seen as locules of air (black color) in the left fronto-parietal region denoted by arrows (Axial section)

Figure 2: Multiple pockets of air seen in the Saggital section marked by arrows demonstrate the Pneumocephalus.
Discussion:
Pneumocephalus is the presence of air in the intracranial cavity. It can be acute ( less than72 hours ) or delayed (more than 72 hours). The most common site is the frontal region (4). Plain skull x-rays can detect Pneumocephalus of about 2 ml, whereas it requires only 0.5 ml of air to be detected by a CT scan (5). Pneumocephalus is most commonly a result of traumatic brain injury, surgical intervention of the brain or infection (5). Trauma accounts for up to 75% percent of the total cases. Chronic infections of ENT especially otitis media also amounts to a number of significant cases. Surgical procedures of brain, spine and ENT like sinus surgery, nasal polypectomy and nasal septum resection accounts for the causes. The incidence after supratentorial craniotomy has been reported to be 100% (6, 7). However, it is very unusual for pneumocephalus to develop post epidural anaeasthesia possibly due to ball valve mechanism in which the air enters the space through the CSF leakage which allows input but not output. Headache post lumbar puncture and epidural anaesthesia is relatively not uncommon but certain situations may demand a more thoughtful approach (3).
In our patient we suspect there was a puncture of the dura during epidural anaesthesia which led to air being trapped and siphoned upwards in an inverted soda bottle fashion. This is supported by the meta-analysis done by Choi et al. which states the incidence of accidental dural puncture in epidural insertion to be 1.5% and among those 52 % will have post puncture headaches (8). In another extensive study performed over ten years, the overall incidence of accidental dural puncture and postdural puncture headache were 0.32% and 0.38%, respectively (9). The authors further stressed that if more than one attempt was required to identify the epidural space, the accidental dural puncture rate increased to 0.91%. In our patient we witnessed the same wherein three attempts were made to identify the epidural space which increased the risk of dural injury and subsequent leaking. Pneumocephalus usually gets absorbed without any clinical manifestations. The conservative treatment involves placing the patient at rest, avoiding Valsalva manoeuver, administering analgesics. With these measures, reabsorption was observed in 85% of cases after 2–3 weeks (5). Use of oxygen mask, nasal catheter, hyperbaric oxygen sessions and good hydration have also been reported. If conservative measures fail to provide the desired results then specific treatment like a epidural blood patch or even surgical closure of the dural gap is indicated (3, 10).
|
Competing Interests None declared Author Details MURTAZA RASHID, M.D, Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. MOHAMMAD ALMOGBIL, M.D, FRCPC, Consultant Pediatric Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. BADER ALOTAOBI, M.D, Consultant Emergency and Disaster Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. MAJID ALJOHANI, M.D, Consultant Emergency Medicine, Royal Commission Hospital, Jubail, Saudi Arabia. CORRESPONDENCE: Dr Murtaza Rashid M.D, Department Of Emergency Medicine, Royal Commission Hospital Jubail, 31961, Saudi Arabia. Email: dr.murtazarashid@gmail.com |
References
- Silva M and Halpern SH. Epidural analgesia for labor: Current techniques. Local Reg Anesth. 2010; 3: 143–153
- Pan PH, Bogard TD, Owen MD. Incidence and characteristics of failures in obstetric neuraxial analgesia and anesthesia: A retrospective analysis of 19,259 deliveries. Int J Obstet Anesth. 2004;13:227–233
- Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgrad Med J. 2006 Nov; 82(973): 713–716
- Solomiichuk VO, Lebed VO, Drizhdov KI. Posttraumatic delayed subdural tension pneumocephalus. Surg Neurol Int. 2013;4:37
- Dabdoub CB, Salas G, Silveira Edo N, Dabdoub CF. Review of the management of Pneumocephalus. Surg Neurol Int 29-Sep-2015;6:155
- Satapathy G.C, Dash HH. Tension Pneumocephalus after neurosurgery in the spine position. Br J Anaes 2000; 84: 115-17
- Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of Pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology 1994; 80: 1008-12
- Choi PT, Galinski SE, Takeuchi L, Lucas S, Tamayo C, Jadad AR. PDPH is a common complication of neuraxial blockade in parturients: A meta-analysis of obstetrical studies. Can J Anaesth. 2003;50:460–469
- van de Velde M, Schepers R, Berends N, Vandermeersch E, de Buck F. Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia department. Int J Obstet Anesth. 2008;17:329–335
- Turnbull D K, Shepherd D B. Post‐dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth 200391718–729

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




