Risk of Development of Osteoporosis due to Depression in the Elderly Individuals: Review Article
Umesh Kumar Vyas
Cite this article as: BJMP 2013;6(2):a612
|
Introduction:
Fifteen percent of elderly individuals report clinically significant depression due to variety of reasons. Osteoporosis is a disorder of bone metabolism which can be caused by multiple factors. The elder population has multiple risk factors for development of low Bone Mineral Density (BMD). Data supports that SSRI causes low BMD. There are numerous mediating processes, factors and causes that may contribute to relationship between depression and low BMD, therefore it has been suggested that depression may be an unrecognized risk factor for development of osteoporosis in this patient population.
Low BMD is a common condition among the elder population; prevalence of osteopenia and osteoporosis is expected to increase due to increasing elder population. Low BMD is associated with increased risk for debilitating fractures, particularly hip, vertebrae and distal forearm. There is a growing body of evidence that depression impact the risk for fractures in the older population.
Most studies support that depression is associated with increased risk for both low BMD and fractures. There are many risk factors for low BMD, but some are unalterable. Therefore it is crucial to identify modifiable risk factors to reduce the public health burden of osteopenia, osteoporosis and fractures, and complications associated with them.
Objective:
A literature review was performed to extract evidence and to evaluate risk of Osteoporosis in depression.
Educational Objectives:
At the conclusion of this article, the reviewer will be able to understand,
- The risk of development of osteoporosis,
- Need for close monitoring and early assessment of risk,
- Need for prophylactic treatment to avoid complications due to development of osteoporosis.
Method:
Pubmed.gov was searched by using pre-determined key word.
Key words:
“Depression AND Osteoporosis"
Background:
Osteoporosis was first recognized as a disorder of bone metabolism in 1947 by Albright. It is the most common degenerative disease in developed countries; it is characterized by low bone mineral density (BMD), causing bone fragility and increased fracture incidence. Over past quarter century, it has emerged as a major public health problem in the Western world, prevalence of osteopenia and osteoporosis is expected to increase dramatically in the next 50 years as the population pyramid shift toward old age. In United States alone, app 10 million individuals over age of 50 have osteoporosis. In addition, 33.6 million Americans in this age group have osteopenia (i.e. a decrease in bone mineral density [BMD] that precedes osteoporosis and its potential complications later in life). The estimated annual fracture rate due to an underlying bone disease is 1.5 million. These fractures lead to pain, skeletal mutilation, disability, loss of independence and increased mortality.1
Low BMD has been shown to be major risk factor for debilitating bone fractures, particularly of the hip, vertebrae and distal forearm.2 The established risk factors for osteoporosis include increasing age, female sex, oestrogen deficiency, glucocorticoid therapy and other medications, smoking, alcohol use, inactivity, and low calcium intake.3 Many prominent risk factors are unalterable, it is therefore crucial to identify modifiable risk factors in order to reduce the public health burden of osteopenia, osteoporosis and the fractures associated with them. In the USA, depression is a common disorder that affects 5 to 9% of women and 1 to 2% men.4 It ranks second only to hypertension as the most common chronic illness encountered in general medical practice.5 This disorder carries a considerable risk of death and is associated with a two to three fold increase in all-cause of non-suicide-related death.6 Fifteen percent of elderly individuals report clinically significant depression.
Definition of Osteopenia and Osteoporosis:
Osteopenia is a condition where bone mineral density is lower than normal, more specifically; it is defined as BMD T-Score between -1.0 and -2.5. It is considered to be precursor to osteoporosis. However, not every person diagnosed with osteopenia will develop osteoporosis. Osteoporosis causes bones to become weak and brittle – so brittle that a fall or even mild stresses like bending over or coughing can cause a fracture.
Osteoporosis-related fractures most commonly occur in the hip, wrist or spine. Bone is a living tissue, which is constantly being absorbed and replaced. Osteoporosis occurs when the creation of new bone does not keep up with the removal of old bone. Osteoporosis affects men and women of all races, but White and Asian women especially those who are past menopause are at highest risk. Medications, dietary supplements and weight-bearing exercise can help strengthen bones.
Literature evidence:
Current evidence supports a bidirectional link between major depressive disorders (MDD), several other mood disorders, and various medical conditions such as osteoporosis and cardiovascular disease.7 A significant association was found between BMD and depressive symptoms after adjustment for osteoporosis risk factors. In Caucasians, depressive symptoms were associated with both osteoporotic and osteopenic levels of BMD.8 A meta-analysis reported BMD is lower in depressed than non-depressed subjects. The association between depression and BMD is stronger in women than men, and in premenopausal than postmenopausal women. Only women psychiatrically diagnosed for MDD display significantly low BMD; women diagnosed by self-rating questionnaires do not.9 Depression is a significant risk factor for fracture in older women.14 Numerous studies have examined association between antidepressant use (both SSRI and TCA) and fracture risk. The majority have found that use of these medications, regardless of class is associated with increased risk of fracture.10 Animal studies have also indicated that serotonin may influence bone mass, particularly during stages of bone growth.11, 12
Daily SSRI (Table 1) use in adults 50 years and older remained associated with a 2-fold increased risk of clinical fragility after adjustment for potential covariates. Depression and fragility fractures are common in this age group, and the elevated risk attributed to daily SSRI use may have important public health consequences.15 (Figure 1). SSRI may increase fracture risk because of their effect on bone physiology and on the risk of falling. Functional serotonin receptors and transporters have been localized to bone, while the administration of SSRI decreases bone mass and strength in growing mice. SSRI function by inhibiting the serotonin transporter. Functional serotonin transporters in osteoblasts, osteoclasts and osteocytes raises the possibility that serotonin transporters may play a role in bone metabolism and those medications that affect this transporter system may also affect bone metabolism. Use of SSRI is associated with an increased rate of bone loss at the hip in this cohort of older women; use of a TCA was not similarly associated with increased rates of hip bone loss in our cohort.16 In men, BMD was lower among those reporting current SSRI use, but not among user of other antidepressants.17 Meta-analysis proved that MDD is associated with low BMD and should therefore be considered a risk factor for osteoporosis. BMD in subjects with MDD was 4.7% lower at the AP spine, 3.5% lower at the total femur, and 7.3% lower at the femur neck as compared to healthy controls.18 NIH meta-analysis concluded MDD was associated with lower BMD at the AP spine, femoral neck and total femur. The deficits in BMD in subjects with depression are of clinical significance and likely to increase fracture risk over the lifetime of these subjects.18
Table 1: List of SSRI (Selective Serotonin Reuptake Inhibitor) and dosages range:
| Generic Name | Brand Name | Dose range |
| Citalopram | Celexa | 10 to 40 mg |
| Escitalopram | Lexapro | 10 to 20 mg |
| Fluoxetine | Prozac | 20 to 80 mg |
| Fluvoxamine | Luvox | 50 to 300 mg |
| Paroxetine | Paxil | 10 to 40 mg |
| Sertraline | Zoloft | 50 to 200 mg |
Figure 1: Fracture-free survival by Selective Serotonin Reuptake Inhibitors (SSRI) use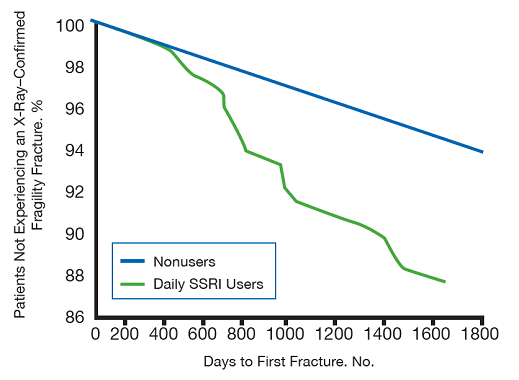
Potential mechanisms of bone loss in depression:
Depression is associated with alterations of the hypothalamic-pituitary-adrenal (HPA) axis at multiple levels, including altered secretion of hypothalamic corticotrophin-releasing hormone (CRH), as indicated by CRH levels in the cerebrospinal fluid, and change in the set point threshold for negative feedback; these changes generally result into hyper-cortisolism.
Pro-inflammatory cytokines are increased in depression and IL-6 is a potent activator of the osteoclast. Oestrogen deficiency in women and androgen deficiency in men may affect bone mass and there is at least theoretical evidence for decreased sexual hormones in both genders during the acute phases of depression. Serotonin transporter receptors are present on the osteoblast and use of antidepressants has been associated with more fractures. Commonly accepted life style risk factors for osteoporosis include smoking, inadequate calcium intake, excessive alcohol intake and physical inactivity.
There are three pathophysiologic pathways leading to low BMD.13 (Figure 2):
- Inadequate acquisition of bone mass early in life
- Elevated resorption of bone mass later in life, and
- Inefficient bone formation during continuous bone remodelling
These pathways are interdependent and the relative importance of each mechanism changes over development and varies by sex.
Figure 2: Pathways linking depression, low bone mneral density and fracture. 13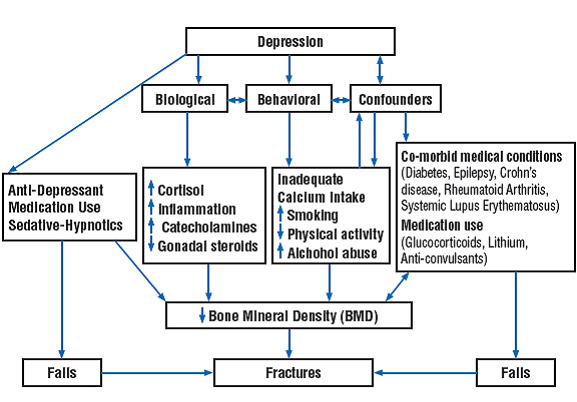
Bottom line:
Current available evidence supports that there is increase of development of osteoporosis due to various factors, pathways and medications used in treatment of depression.
Conclusion:
Major depressive disorder is an important but still unrecognized risk factor for osteoporosis. Depression should be considered as an important risk factor for osteoporosis. Depression is associated with low BMD, with a substantially greater BMD decrease in depressed women and in cases of clinical depression. These patients need close monitoring, early assessment of risk and preventive measures to avoid complications. Premenopausal women with major depression should undergo DXA screening. Similar recommendation may be made for postmenopausal women with depression especially in the presence of one or more known risk factors for development of osteoporosis.
Once a diagnosis of osteoporosis is made in subjects with major depression, DXA measurements should be performed with a frequency based on the current WHO algorithm; this model takes into account the presence of other risk factors and age of the subjects.
Clinical Point:
Periodic BMD measurements and anti-osteoporotic prophylactic and curative measures are strongly advocated for these patients.
|
Competing Interests None declared Author Details UMESH KUMAR VYAS, M.D., Chair of Department of Psychiatry, Medical Director of In-Patient Behavioral Health Unit, Regional Medical Director of Sleep Disorders Center, Psychiatrist and Sleep Disorders Specialist, Mayo Clinic Health System, Mankato, MN, USA; Adjunct Clinical Assistant Professor, Department of Family Medicine and Community Health, University of Minnesota, Minneapolis, MN, USA; Adjunct Assistant Professor of Psychiatry and Sleep Medicine, College of Osteopathic Medicine, Des Moines University, Des Moines, IA, USA. CORRESPONDENCE: UMESH KUMAR VYAS, M.D., 1025 Marsh Street, P O Box 8673, Mankato, MN, 56002-8673, USA. Email: Vyas.umesh@mayo.edu |
References
- US Department of Health and Human Services: Office of the Surgeon General: Bone Health and Osteoporosis: 2004; A Report of the Surgeon General. Available at http://www.surgeongeneral.gov/library/bonehealth/. Accessed December 1, 2008.
- Cummings SR, Black DM, Nevitt MC, et al. The study of osteoporotic fractures research group. Appendicular bone density and age predict hip fracture in women. JAMA, 1990; 263(5):665-668
- Ross PD. Osteoporosis. Frequency, consequences, and risk factors. Arch Intern Med, 1996; 156(13):1399-1411
- Robins LN, Helzer JE, Weissman MM, et al. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry, 1984; 41(10):949-958
- Wells KB, Stewart A, Hays RD et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA, 1989; 262(7):914-919
- Zheng D, Macera CA, Croft JB et al. Major depression and all-cause mortality among white adults in the United States. Ann Epidemiol, 1997; 7(3):213-218
- Evans DL, Charney DS, Lewis L et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry, 2005; 58:175-189
- John Robbins, Calvin Hirsch, Rachel Whitmer et al. The association of bone mineral density and depression in an older population J Am Geriatric Soc, 2001; 49(6):732-736
- Itai A. Bab, Raz Yirmiya. Depression and bone mass Ann N Y Acad Sci, 2010; 1192:170-175
- Takkouche B. Montes-Martinez A, Gill S et al. Psychotropic medications and the risk of fracture: a meta-analysis. Drug safety, 2007; 30:171-184
- Bliziotes M, Gunness M, Eshleman A et al. The role of dopamine and serotonin in regulating bone mass and strength; studies on dopamine and serotonin transporter null mice. J Musculoskele Neuronal Interact, 2002; 2:291-295
- Warden S, Robling A, Sanders M et al. Inhibition of the serotonin (5-hydroxytryptamine) transporter reduces bone accrual during growth. Endocrinology, 2005; 146:685-693
- B Mezuk, W. W. Eaton, S. H. Golden. Depression and osteoporosis: epidemiology and potential mediating pathways. International Osteoporosis Foundation and National Osteoporosis Foundation, 2007
- M A Whooley, K E Kip, J A Cauley et al. Depression, falls, and risk of fracture in older women, Arch Intern Med, 1999; 159:484-490
- J B Richards, A Papaioannou, J D Adachi et al. Effect of selective reuptake inhibitors of the risk of fracture. Arch Intern Med, 2007; 167:188-194
- S J Diem, T L Blackwell, K L Stone et al. Use of antidepressants and rates of hip bone loss in older women. Arch Intern Med, 2007; 167:1240-1245
- E M Haney, B K S Chan, S J Diem et al. Association of low bone mineral density with selective serotonin reuptake inhibitor use by older men. Arch Intern Med, 2007; 167:1246-1251
- G. Cizza, S. Primma, M. Coyle et al. Depression and Osteoporosis: A research synthesis with Meta-analysis. Horm Metab Res, 2010; 42(7):467-482

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




