Successful Anaesthetic Management of an Intra-tracheal Tumour
Harshal D Wagh
Cite this article as: BJMP 2015;8(1):a808
|
|
Abstract We report a successful management of an intra-tracheal tumour in a 56 year old patient. The tumour was situated about 4 cm above the carina.The case was managed without the need of cardiopulmonary bypass. An orotracheal tube placed above the tumour was used to ventilate the lungs before the trachea was opened. A smaller tube was placed in the left bronchus to ventilate the left lung after the trachea was opened to facilitate sleeve resection and anastomosis of the trachea. The patient was extubated in the immediate postop period without any adverse effects. Careful preoperative planning and good team work made the procedure possible and without complications. |
INTRODUCTION
Anaesthetic management of a patient with a tracheal tumour is challenging, as the airway is shared with the surgeon and patency must be maintained despite airway manipulation.
Several anaesthetic techniques have been used in patients requiring tracheal resection and reconstruction. Cardiopulmonary bypass standby after femoral artery and vein cannulation and then intravenous/inhalational induction while oxygenating the patient has been considered to be a reasonable approach. Intratracheal tumours are challenging to anaesthetists because of the difficulty in establishment of a patent airway before commencement of surgery. The principal anaesthetic consideration is ventilation and oxygenation in the face of an open airway.
CASE REPORT
A 56 year old male with no other co-morbidities presented to the Thoracic Oncology department with a history of progressive dyspnoea and orthopnoea.On examination he was found to have dyspnoea at rest and could not complete full sentences while talking. Change of position made no difference to his symptoms.
Routine blood investigations which included full blood count, renal and liver functions, coagulation profile, ECG and 2DEcho were within normal limits. PFT showed a typical intrathoracic obstructive picture.
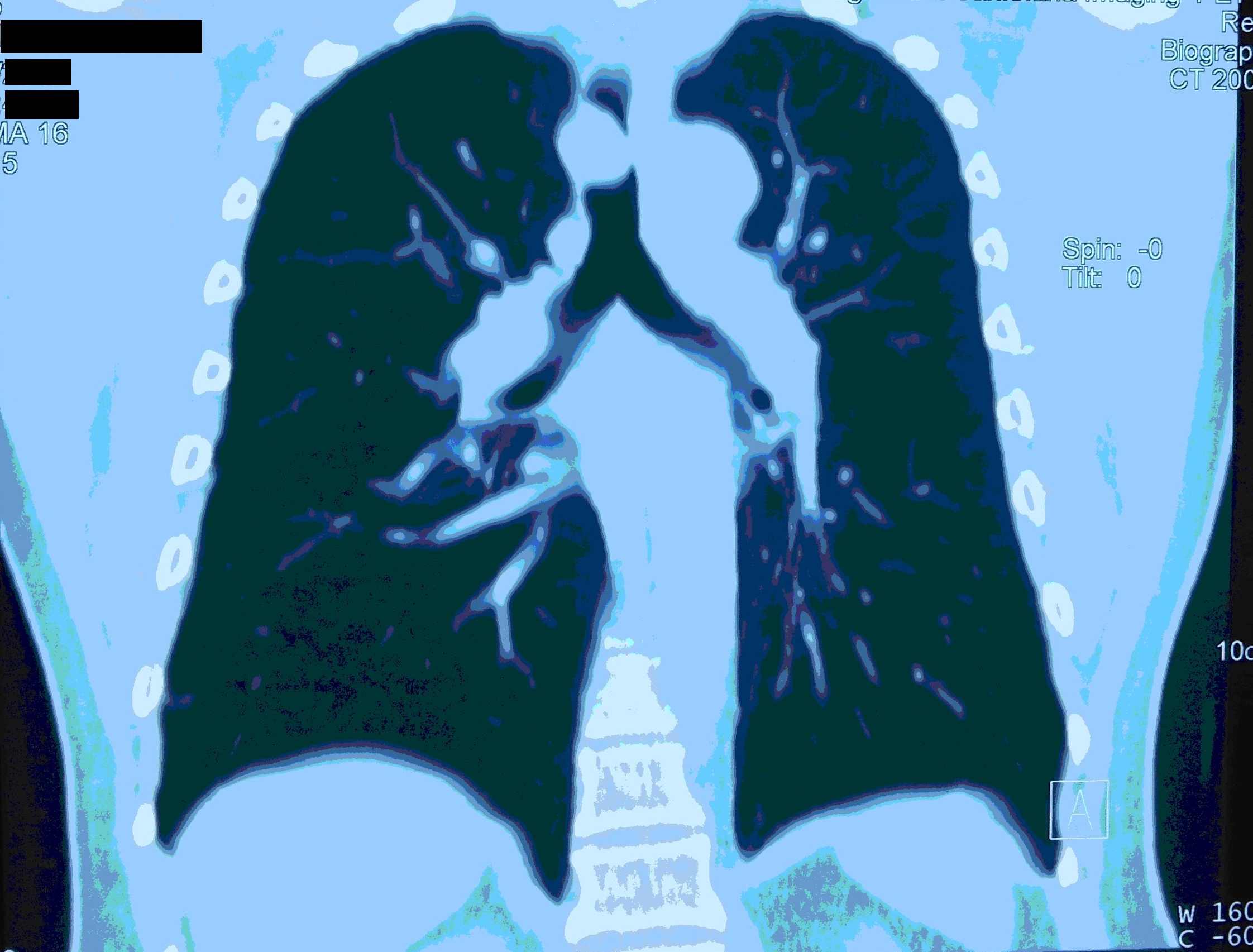
His chest X-ray showed bilateral hyperinflated lungs suggesting airtrapping. CT of the chest showed an intratracheal growth about 4 cm above the carina almost completely obstructing the lumen. An awake flexible bronschoscopy confirmed the CT scan findings. A 2.7mm flexible bronschocope was passed with difficulty beyond the tumour to visualise the carina. Excision of the intratracheal tumour was planned with possible resection and anastomosis of the involved tracheal segment. A careful perioperative plan was discussed and decided in agreement with the thoracic surgeons, anaesthetist, cardiovascular surgeons and the rest of the team members.
Flexible and rigid bronchoscope, a Sanders venturi, an additional anaesthesia machine and various sizes of reinforced and normal endotracheal tubes and tracheostomy tubes were kept ready.
Preoperatively the patient had incentive spirometry and bronchodilator nebulisation and intravenous steroids. An awake epidural at T9-10 level and radial artery cannulation were done under local anaesthesia without any problems. Two 16 gauge peripheral IV lines were sited under local anaesthesia.
After adequate preoxygenation anaesthesia was induced with IV propofol along with oxygen and sevoflurane with BIS monitoring. As mask ventilation proved to be easy the patient was paralysed with suxamethonium. There was no difficulty in ventilation after muscle paralysis. An 8.5 number COETT portex tube was placed in the trachea with the cuff just beyond the cords to avoid possible trauma to the tumour. Since there was preoperative evidence of airtrapping, ventilator settings were set to an I:E ration of 1:3 with a tidal volume of 550ml, respiratory rate of 12-14 per minute and PEEP of 4. At these ventilator settings the airway pressures were reaching up to 22 cm of H20 and ETCO2 reaching a maximum of 40mmHg. Anaesthesia was maintained with oxygen: air with sevoflurane and atarcurium for muscle paralysis.
Flexible bronchoscopy was done to confirm the position of the endotracheal tube, which showed that the ETT was adequately above the tumour.
A laryngeal drop procedure was done in the supine position with neck extension to facilitate mobilisation of the trachea for resection anastomosis. After the laryngeal drop procedure a right thoracotomy was done in the left lateral position. At this point of the procedure, the patient was ventilated with low tidal volumes of 300 and respiratory rate of 16-20 to keep the ETCO2 at around 40.The right lung was surgically retracted and the trachea was exposed up to the carina. A repeat bronchoscopy was done through the ETT to help identify the upper and lower extent of the tumour. The trachea was then opened below the tumour, after which a 6.5 reinforced tube was introduced through the left bronchus to aid ventilation of the left lung. This ETT was withdrawn intermittently to help visualisation and aid surgical excision of the tumour and sleeve resection of the trachea. The left lung was ventilated till partial closure of the trachea. The left-sided tube was then removed. Ventilation resumed through the orotracheal tube with intermittent occlusion of the defect with gauze by the surgeon. The orotracheal tube was adjusted under vision before closure of the trachea to position it above the anastomotic site. The trachea was sutured and the thoracotomy incision closed without any adverse event. The neck was kept in a flexed position to avoid tension on the tracheal anastomotic area.
The patient was then extubated in the immediate postoperative period without any problems and the recovery was uneventful.
DISCUSSION
Anaesthetic management of a patient with a tracheal tumor is challenging, as the airway is shared with the surgeon, and patency must be maintained despite airway manipulation1, 2. Several anaesthetic techniques have been used in patients requiring tracheal resection and reconstruction 3–5.
Primary tracheal masses are very rare and mostly malignant, occurring in 0.2 in 1,00,000 persons per year 6 and among these squamous cell carcinomas form the main bulk. Cardiopulmonary bypass standby after femoral artery and vein cannulation and then intravenous/inhalational induction while oxygenating the patient with the oxygen inhalation has been considered to be a reasonable approach 7. Byrne JG et al (2004) advocated planned use of CPB to facilitate complete resection of thoracic malignancies after careful patient selection 8.
These patients are often mistaken to have asthma and require treatment with inhaled corticosteroids and beta agonists 9. They are generally treated for many years for asthma or COPD, unless a CT scan or endoscopic procedure is done for the symptoms 10. Intratracheal masses usually start getting symptomatic when 75% or more of the tracheal lumen is obstructed. Tracheal lesions present at lower level can have more complicated management of airway, anaesthesia and surgery for successful and safe removal of the mass. 10
Intratracheal tumours are challenging to anaesthetists because of the difficulty in establishment of a patent airway before commencement of surgery. The principal anaesthetic consideration is ventilation and oxygenation in the face of an open airway. Ventilation can be managed in many ways, including manual jet ventilation, high frequency jet ventilation, distal tracheal intubation, tracheostomy, spontaneous ventilation and CPB.11
Knowledge of various techniques available for management of such cases is vital. In order to have a successful and safe outcome it is extremely important to have good communication between the anaesthetic, surgical and intensive care team.
The challenge in managing such cases lies in establishing and maintaining a patent airway and also preventing seepage of blood and tumour particles distally into the tracheobronchial tree during the surgery.
There is a possibility of total airway obstruction during ventilation attempts using positive pressure because airway obstruction has a fixed and dynamic component. Dislodgement of the tumour, possibly from trauma following intubation causing total obstruction, should also be considered.
Thus an intratracheal tumour was successfully removed without any complications and by avoiding CPB. This case report also highlights the importance of proper planning and good communication between team members to ensure a successful and safe outcome.
|
Acknowledgements RAJESH MISTRY, Consultant and Head of the Department of Oncosurgery, Kokilaben Ambani Hospital, Mumbai, India. Competing Interests None declared Author Details DR.HARSHAL D WAGH, MBBS,DA,DNB,FCPS,FRCA(LON), Kokilaben Ambani Hospital, Mumbai, India. CORRESPONDENCE: DR HARSHAL WAGH, Kokilaben Ambani Hospital, Andheri, 4 Bungalows, Mumbai, 400053,INDIA. Email: drhdw@yahoo.com |
References
- Licker M, Schweizer A, Nicolet G, et al.Anaesthesia of a patient with an obstructing tracheal mass: a new way to manage the airway. Acta Anaesthesiol Scand 1997;41:84–6.
- Furimsky M, Aronson S, Ovassapian A.Perioperative management of a patient presenting for resection of a tracheal mass. J Cardiothorac Anesth 1998;12:701–4.
- Divatia JV, Sareen R, Upadhye SM, et al.Anaesthetic management of tracheal surgery using the laryngeal mask airway.Anaesth Intensive Care 1994;22:69 –73.
- Kawaraguchi Y, Taniguchi A. Anesthetic management of a 9-year-old child undergoing resection of a tracheal tumor. Paediatr Anaesth 2005;15:512– 4.
- Mentzelopoulos SD, Romana CN, Hatzimichalis AG, et al. Anesthesia for tracheal resection: a new technique of airway management in a patient with severe stenosis of the midtrachea. Anesth Analg1999;89:1156–60.
- Azar T, Abdul-Karim FW, Tucker HM: Adenoid cystic carcinoma of the trachea. Laryngoscope 1998, 108(9):1297-300.
- Céline Pinsonneault, Joanne Fortier, François Donati: Tracheal resection and reconstruction. Can J Anesth 1999, 46(5):439-455.
- Byrne JG, Leacche M, Agnihotri AK, Paul S, Bueno R, Mathisen DJ, Sugarbaker DJ: The use of cardiopulmonary bypass during resection of locally advanced thoracic malignancies: a 10- year two-center experience. Chest 2004, 125(4):1581-6.
- Jones TM, Alderson D.Sheard JD,Swift AC.Tracheal paraganglioma: A diagnostic dilemma culminating in a complex airway management problem.J Laryngol Otol 2001;115:747-9.
- Azorin J, Lamberto JF, Personne C, Larmignat P, Khellaf M, Lmeny JL,et al. Adenoid cystic carcinoma of the trachea: Treatment by combined laser therapy and surgery.Rev Mal respire 1987;4:95-6.
- Pinsonneault C, Fortier J, Donati F. Tracheal resection and reconstruction.Can J Anaesth 1999;46:439-55

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




