Synchronus paraspinal and hepatic hydatid disease ; a rare presentation
Ashish S Motewar, Sayalee S Narwade and Mandar R Tilak
Cite this article as: BJMP 2012;5(4):a539
|
|
Abstract Hydatid cystic disease is a common zoonotic infection in the Indian subcontinent. However in the following case we report a rare presentation found in a young patient synchronously in the paraspinal and intrahepatic location without intercommunication. A high index of clinical suspicion is necessary for diagnosis. Hydatid disease is to Echinococcus species commonly granulosus, sometimes multilocularis. The common locations of hydatid cysts are the liver (65% to 75%) and lungs (25%-30%). Hydatid disease rarely develops in locations such as spleen, kidney, bones, heart, brain, peritoneum, myocardium and muscles (1-4%). A 25 year old male presented with complaining of backache on the right and fullness in the right paraspinal region. On clinical examination he had a non ballotable lump in right paraspinal region within intra muscular plane extending from posterior subcostal margin to iliac region. CT abdomen (P+C) revealed a well defined hypodence non-enhancing cystic lesion in the right lobe of the liver with peripheral calcification with lesion of similar morphology in right paraspinal muscles. Exploration of the right paraspinal region was done. Cyst was beneath the oblique & lattisimus dorsi, superficial to psoas muscle without invasion in it. Cyst opened multiple daughter cysts along with pus evacuated. Cyst excised in totto without spillage. Hydatid cyst is frequently asymptomatic, most prevalent in sheep and cattle-breeding areas. The cysts can not easily grow in muscles due to their contractility and lactic acid content. The latent period of cyst development varies between 5-20 years. Surgery is the optimal treatment for hydatid cysts. Open cyst evacuation is indicated for gharbi types 4&5, posterior cysts, central cysts, more than 3 cysts, infected cysts, biliary communication, pulmonary communication & peritoneal rupture. Alternative therapy with non-toxic scolocidal agents or combination chemotherapy has been advocated in the management of recurrence and high risk of contamination. |
Introduction
Hydatid disease is due to Echinococcus species commonly granulosus sometimes multilocularis. The common locations of hydatid cyst are the liver (65% to 75%) and lungs (25%-30%) 1,2,3. Hydatid disease rarely develops in some locations such as the spleen, kidney, bones, heart, brain, peritoneum, myocardium and muscles (1-4%)1. In our review of literature, concomitant paraspinal and intrahepatic hydatid is reported rarely.
Case Report
A 25 year old male presented with backache on the right for 1 month and fullness in the right paraspinal region. No history of trauma, fever, burning micturition, pain in abdomen, weight loss or hematuria.
On clinical examination he had non ballotable lump in the right paraspinal region, measuring 15x5x5cm with ill defined margins intra muscular plane extending from the posterior subcostal margin to the iliac region with no overlying skin changes and no organomegaly.
Blood investigations including liver function tests and kidney function tests were normal. Ultrasound examination revealed hepatomegaly with thick walled cystic lesion in the right lobe of the liver and the in muscle plane in the right renal angle region.
CT abdomen (P+C) revealed a well defined hypodence non-enhancing cystic lesion measuring 45x40 cm seen in the right lobe of the liver with peripheral calcification with another lesion of similar morphology of size 14x5x3.6cm in the right paraspinal muscles with no intercommunication between them and no bone, spinal canal alteration or compression of the right kidney.
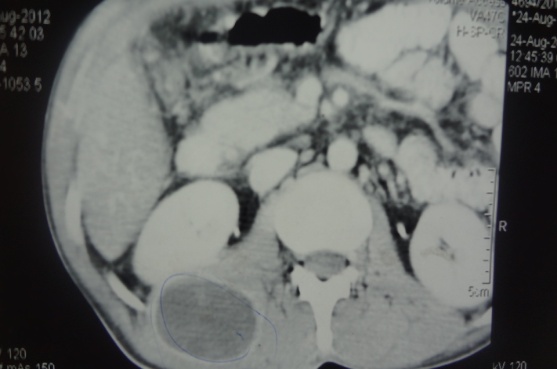
Figure 1: Right paraspinal hydatid
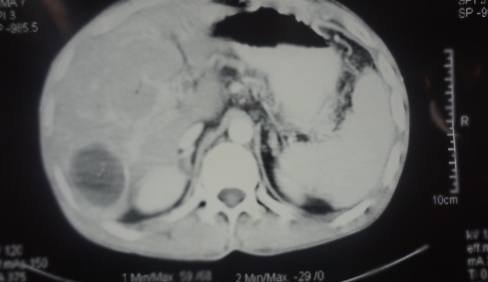
Figure 2: Intrahepatic hydatid
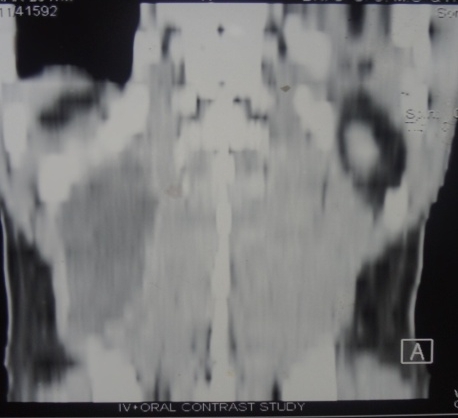
Figure 3: Coronal view of CT image
The diagnosis of paraspinal hydatid cyst was confirmed. As the patient was symptomatic for paraspinal hydatid cyst only and the size of the hepatic cyst was small, exploration of the right paraspinal region was done after 21 days of antiscolicidal treatment. There was a cyst measuring 15x5x5 cm beneath the oblique and lattisimus dorsi ,superficial to the psoas muscle without invasion into it .The cyst opened multiple daughter cysts along with pus evacuated. The cyst excised in totto without rupture & spillage. Negative suction drain was kept. Post operatively on day 3 the drain was removed, stitches removed on day 10 and discharged. Histopathology confirmed diagnosis.

Figure 4: Intraoperrative photograph

Figure 5: Photograph of multiple daughter cysts
Discussion
Hydatid disease is most prevalent in sheep and cattle-breeding areas, which is where the first step in the chain of transmission occurs. The causative agent is introduced to the dog (the primary host) through the faeces of livestock. The minute larval form of E. granulosus lives in the small intestine of the dog species. The eggs are passed in the faecesof an infected dog and can be transferred to mammal (man – intermediate host) that ingests them. After ingestion, the embryos are released from the eggs, traverse the intestinal mucosa and disseminate systemically via venous and lymphatic channels and develop into hydatid cysts in various body parts.
The cysts cannot easily grow in muscles due to their contractility and lactic acid content. The wall of a cyst in the muscle is formed by three layers: the inner germina, intermediate and outer granulomatous adventitial layer. The most common skeletal sites include hip, thigh, shoulder and humerus regions. Hydatid cysts are frequently asymptomatic1. The latent period of cyst development varies between 5 and 20 years4,5.
Serological tests are widely used to diagnose hydatid cysts. However, positive serological results do not confirm, nor negative results exclude the disease1,6. The imaging features of hydatid cysts are well described in the literature. Ultrasound scans are a sensitive, safe, non-invasive method. It is the procedure of choice for the diagnosis of cysts with a “honeycomb” pattern (type 3), as observed in our patient. Gharbi’s classification provides morphological description on ultrasound. Type 1-pure fluid collection, type 2-fluid collection with split wall (floating membrane), type 3-fluid collection with septa, type 4-heterogenous echographic pattern, type 5-reflecting thick walls.
As seen in our case the cyst fluid appears anechoic at USS, yields an attenuation value of 3-30HU at CT. Calcifications in the cyst wall as in our case are best detected on CT scans. CT has the advantage of detecting smaller cysts when located outside the liver and sometimes differentiating parasitic from non-parasitic cysts, for follow-up studies during chemotherapy. Other diagnostic means such as fine needle aspiration should be avoided because of dangerous anaphylactic reactions7.
Surgery is the optimal treatment for hydatid cyst. Open cyst evacuation is indicated for gharbi types 4 & 5, posterior cysts, central cysts, more than 3 cysts, large cysts, heavy calcification, infected cysts with above criteria, biliary communication, pulmonary communication and peritoneal rupture. Laparoscopic evacuation is indicated in Gharbi type 1 or 2, anterior cysts, peripheral cysts,1-3 cysts, small cysts, no or minimal calcification. Pericystectomy is complete resection of cyst wall without entering the cyst cavity.
Alternative therapy with non-toxic scolocidal agents or combination chemotherapy using imidazole derivatives, particularly albendazol, has been advocated in the management of patients with recurrence and high risk of contamination8.
|
Competing Interests None declared Author Details ASHISH S MOTEWAR, Associate Professor, Dept. Of Surgery, Government Medical College, Nanded, India. SAYALEE S NARWADE, Resident, Dept. Of Surgery, Government Medical College, Nanded, India. MANDAR R TILAK, Assistant Professor, Dept. Of Surgery, Government Medical College, Nanded, India. CORRESPONDENCE: Dr.SAYALEE S NARWADE, P.G.Hostel, Dr.SCGMC,Vazirabad, Nanded, India. 431601 Email: mailme.drsayaleenarwade@rediffmail.com |
References
- Garcia-Diez A.I., Ros Mendoza L.H.,Villacampa V.M. et al.: MRI evaluation of soft tissue hydatid disease. Eur Radiol,2000, 10: 462-466.
- White C Jr, Weller PF. Echinococcosis. In: Braunwald E, FauciAS, Kasper DL, Longo DL, Jameson JL eds Harrison’s Principles of Internal Medicine 15th edition. McGraw Hill; 2001; p.1250.
- Tatari H, Baran O, Anlidag T, et al. Primary intramuscular hydatidosis of supraspinatus muscle. Arch Orthop Trauma Surg.2001;121: 93–948.
- Berrada S., Ridai M., Mokhtari M.: Kystes Hydatiques de la rate: splénectomies ou chirurgie conservatrice Ann Chir, 1991, 45: 434.
- Bellakhdar A., Lamhamdi A.,Touzani K.et al.: Les kystes hydatiques de la rate (25 cas). J Chir,1986,.123: 326.
- Akhan O., Ensari S., Özmen M.:Percutaneos treatment of a parotid gland hydatid cyst: a possible alternative to surgery. Eur Radiol, 2000,12: 597-599.
- Essaki.o; Hajjam M., Kadiri R; hydatique des parties molles; aspects radiologiques: annals of radio 1996
- Akal M., Kara M.: Primary hydatid cyst of the posterior cervical triangle. J Laryngol Otol, 202, 116: 153-155.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




