An Unusual Presentation of Left Ventricular Free Wall Rupture following a Silent Myocardial Infarction
Andrew Peter Vanezis, Rehan Quadery, Mohammad Wasil and Mohammed Azher
Cite this article as: BJMP 2009:2(1) 41-43
|
Abstract
Left ventricular free wall rupture is a serious complication of myocardial infarction (MI) with a mortality rate without intervention close to 100%. Its presentation is classically late following an MI but in some cases can present within 24 hours. There can be sudden overt clinical symptoms or it can present insidiously and therefore there must be a high index of suspicion. This report highlights the case of a gentleman with no prior history of ischaemic heart disease that presented with non-specific symptoms. A diagnosis of left ventricular (LV) free wall rupture near the atrial appendage, post MI was made and he was managed successfully.
Clinical Presentation
We present the case of a 75 year old gentleman who collapsed suddenly whilst riding his bicycle. According to an eye-witness he was unresponsive & confused for a few minutes after the episode. Paramedics attended and brought him to the Accident and Emergency department at a local hospital and he was subsequently transferred to the Admissions Unit. Initially he was confused with no recollection of the collapse however his confusion abated after a short period of time.
He was normally fit and well, his only past medical history of note being chronic neck pain requiring simple analgesia and mild asthma requiring when necessary salbutamol inhalers. He was however a life-long smoker with a minimal alcohol intake.
On arrival to the hospital, the patient was conscious, oriented, afebrile and not in any pain. His Glasgow Coma Scale (GCS) was 15/15, pulse was 92/min, regular but weak and the right radial and femoral pulses were absent. His systolic blood pressure was 55mmHg in the right arm and 105mmHg in the left arm. The only other positive finding on examination was muffled heart sounds. Bloods were taken and results are shown in Table 1 with normal ranges given for reference (results within normal limits are not shown).
|
Random Blood Glucose |
16 mmol/l |
<11.1 mmol/l |
|
Troponin I (12 hour) |
6.16 ng/ml |
<0.04 ng/ml |
|
WBC |
14.0 x109/l |
4-11 x109/l |
|
CRP |
179 mg/l |
<10 mg/l |
|
Hb |
10.9 g/dl |
13-18 g/dl (men) |
Table 1. Blood results with normal ranges in italics.
In view of the high blood glucose and history of collapse, the patient was aggressively treated with insulin and intravenous fluids. However after receiving 2 litres of intravenous fluids, there was no haemodynamic response. An arterial blood gas on air was performed and the results are shown in Table 2 with normal ranges given for reference.
|
pH |
7.40 |
(7.35-7.45)) |
|
pCO2 |
3.0 Kpa |
(4.7-6.0 Kpa) |
|
pO2 |
14.8 Kpa |
(10.8-12.5 Kpa) |
|
HCO3 |
13.6 mmol/l |
(22-28 mmol/l) |
Table 2. Arterial Blood Gas with normal ranges in italics.
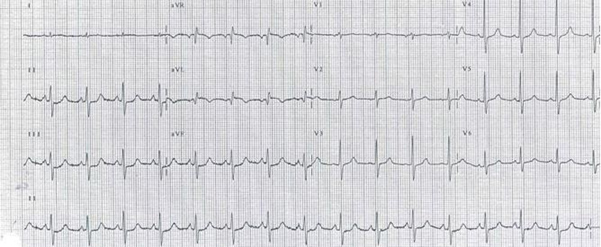
A Chest X-ray was performed and showed nothing unusual. However an ECG demonstrated ST depression in the inferior leads & T- wave inversion with a Q wave in aVL (see figure 1). Differential diagnosis at this stage was therefore aortic dissection, carotid dissection and left ventricular wall rupture (post myocardial infarction).
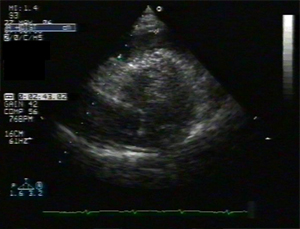
A subsequent CT scan showed no aortic dissection, but probable haemopericardium together with an occluded right common iliac artery (see figure 2). Trans-thoracic echocardiogram confirmed haemopericardium with no suggestion of tamponade (see figure 3) and in addition demonstrated some mild LV diastolic dysfunction. CT scan of the brain and the carotids showed no evidence of carotid dissection but did indicate significant stenosis of the right subclavian artery. The diagnosis of left ventricular free wall rupture was made at this juncture. It was noted that the variability in blood pressure between both arms and between upper limbs and lower limbs was exacerbated by coincidental stenosis in the right common iliac and right subclavian arteries which possibly delayed diagnosis.
Subsequent coronary angiogram showed a blocked intermediate coronary artery (a branch of the left main coronary artery), 2 stenosed areas in the left anterior descending coronary artery (LAD) and a 50% occlusion of the right coronary artery (RCA). Later a trans-oesophageal echocardiogram (TOE) demonstrated separation of the ventricular free wall between the LAD artery and the left atrial appendage, high up in the heart a very unusual position indeed. The diagnosis of Left Ventricular Free Wall Rupture following a Silent Myocardial Infarction was therefore confirmed. The patient was transferred to a nearby cardiac surgery centre and an emergency patch repair of the ventricular free wall rupture was performed.
Figure 1. ECG demonstrating ST depression in II, III and aVL & T-wave inversion with a Q wave in aVL.
The patient had a prolonged recovery, spending 2 weeks on the Cardiac ICU and then subsequently developed hospital acquired pneumonia and remained an inpatient on a general medical ward for a further 4 weeks where he made slow progress. He later spent 4 weeks in a rehabilitation centre before finally returning home.
Figure 2. Thoracic CT with obvious haemopericardium.
Figure 3. Transthoracic echo with evidence of pericardial fluid.
Discussion
First described by William Harvey in 1647, left ventricular (LV) free wall rupture is a dramatic complication of myocardial infarction where there is a rupture of infarcted LV free wall tissue. The rupture is commonly insidious with bleeding into the pericardial sac and subsequent cardiac tamponade. It is hard to assess as clinical and autopsy results vary considerably. It contributes to nearly 15% of deaths due to acute MI1, with the average age of those affected being 69 years. It is third only to cardiogenic shock and arrhythmias as the leading cause of death following a myocardial infarction.2 Hutchins et al reviewed 153 post mortem results with gross and histological evidence of acute myocardial infarction and reported that 30.7% of patients in this group who had died from sudden death had a cardiac rupture.3 It is more common in females and classically occurs 3 to 6 days post MI, however in some studies, up to 50% of cases have been reported less than 24 hours post MI.4There is a history of previous MI in 25% cases but often LV free wall rupture can be the first presentation of ischaemic heart disease.5 Around 50% of the cases of LV free wall rupture are due to anterior MIs with LAD involvement.6There is a new murmur in 25% cases and echocardiography may often demonstrate a pericardial effusion. The prior use of NSAIDS and corticosteroids and a presentation which may mimic major artery dissection often delays thrombolytic therapy.
Unfortunately the current mortality rate in the UK is around 90%. Of note the incidence of LV free wall rupture post MI has increased since the more widespread availability of coronary care units and it is thought that this is because more people are now surviving the first few days post MI.7
The pathophysiological process involves thinning of the myocardial wall with the intensity of necrosis occurring at the terminal end of the vessel (watershed area) where there is often poor collateral flow. The shearing effect of myocardial contraction against a stiffened necrotic area causes rupture. The most common rupture location is on the anterior or lateral wall of the left ventricle.8 A midventricular position along the apex to base axis is most common. It can present either with sudden death or can present sub acutely e.g. with nausea, hypertension or pericardial type chest discomfort or pain. The gentleman discussed in this report collapsed with no preceding symptoms and as mentioned the location of his rupture was in a very unusual place, high up near the atrial appendage.
Transoesophageal echo (TOE) is diagnostic for this condition and is the gold standard.9 However it is found to have only a 70% sensitivity rate for LV free wall rupture10 and therefore some centres advocate the use of cardiac MRI when available.11 Initial management is haemodynamic stabilization and this is often followed by blood transfusion, pericardiocentesis12, inotropic support and the use of an intra-aortic balloon pump but ultimately prompt surgical repair is required.
Various surgical techniques have been applied including suturing of the infarcted ventricle but modern surgical repair involves the application of a Teflon felt patch over the ruptured area with a synthetic biocompatible glue (e.g. cyanoacrylate) as an adhesive to keep the patch attached to the epicardium.13,14 Crucially it can be performed without the use of cardiopulmonary bypass in most of cases. The current overall operative mortality for surgical intervention is reported to be around 24-35%15.
Ultimately survival depends on early recognition of the condition, prompt investigations & diagnosis and urgent surgical treatment. Unfortunately at the present time the condition is usually diagnosed at post-mortem.
Conclusion
The patients presentation i.e. collapse with no proceeding symptoms coupled with the fact that he was suffering a silent MI with no prior indications of ischaemic heart disease e.g. angina, shortness of breath etc and the rapid subsequent development of left ventricular free wall rupture in such an high position made this quite an unusual case. Stenosis in the right common iliac and subclavian arteries did delay diagnosis slightly, as aortic and carotid dissection had yet to be ruled out but ultimately this patient survived probably because of early diagnosis despite these obstacles and subsequent prompt treatment.
COMPETING INTERESTS
None Declared
AUTHOR DETAILS
ANDREW PETER VANEZIS MBChB BSc, FY2 Doctor, Barts and The London NHS Trust, UK.
REHAN QUADERY MBBS, ST3 Medicine, Bedford Hospital NHS Trust, UK
MOHAMMAD WASIL PhD, Assistant Director of Research & Development, Bedford Hospital NHS Trust, UK
MOHAMMED AZHER FCCP FRCP, Consultant Chest Physician, Bedford Hospital NHS Trust, UK
CORRESPONDENCE: REHAN QUADERY, Bedford Hospital NHS Trust, UK
Email: rehan.quadery@bedfordhospital.nhs.uk
References
-
Wehrens XH, Doevendans PA. Cardiac rupture complicating myocardial infarction. Int J Cardiol. 2004;9:285-292
-
Pohjola-Sintonen S, Muller JE, Stone PH, Willich SN, Antman EM, Davis VG, Parker CB, Braunwald E. Ventricular septal and free wall rupture complicating acute myocardial infarction: experience in the Multicenter Investigation of Limitation of Infarct Size. Am Heart J. 1989;117:809818
-
Hutchins, Kenneth D, Skurnick, Joan, Lavenhar, Marvin, Natarajan, Geetha A. Cardiac Rupture in Acute Myocardial Infarction: A Reassessment. American Journal of Forensic Medicine & Pathology. 23(1):78-82, March 2002.
-
Becker AE, Anderson RH. Cardiac pathology. An integrated text and colour atlas. London: Gower Medical Publishing; 1983.
-
Shirani J, Berezowski K, Roberts WC. Out-of-hospital sudden death from left ventricular free wall rupture during acute myocardial infarction as the first and only manifestation of atherosclerotic coronary artery disease. Am J Cardiol 1994 Jan; 73(1): 88-92
-
Slater J, Brown RJ, Antonelli TA, et al. Cardiogenic shock due to cardiac free-wall rupture or tamponade after acute myocardial infarction:A report from the SHOCK trial registry. J Am Coll Cardiology. 2000;36:1117-1122
-
Reddy SG, Roberts WC. Frequency of rupture of the left ventricular free wall or ventricular septum among necropsy cases of fatal acute myocardial infarction since introduction of coronary care units. Am J Cardiol 1989;63:90611
-
David, TE. Surgery for post infarction rupture of the free wall of the ventricle. In: David TE. , editor. Mechanical Complications of Myocardial Infarction. Austin, R.G. Landes Company; 1993. p. 142.
-
Cheitlin, MD et al. ACC/AHA/ASE 2003 Guideline update for the clinical application of echocardiography. J Am Coll Cardiol. 2003;42:95470
-
Lopez-Sendon J, Gonzalez A, Lopez de Sa E, Coma-Canella I, Roldan I, Dominguez F, et al. Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specificity of clinical, hemodynamic and echocardiographic criteria. J Am Coll Cardiol 1992;19: 114553.
-
Rajiv Agarwal, Pedro Diaz-Ortiz, Ravinder Reddy, Veronica Lenge, R. David Fish, David A. Ott, John Connelly, and Scott D. Flamm. Asymptomatic Incomplete Left Ventricular Apical Rupture Diagnosed by Cardiac Magnetic Resonance Imaging. Tex Heart Inst J. 2006; 33(1): 9395
-
Rolf Svedjeholma, Erik Hkansonb, Mrten Lindstrmc and Per Hjort. Case report - Cardiac general. Post-infarct left ventricular free wall rupture and ventricular septal defect managed by pericardial aspiration during transport to referral hospital. Interactive Cardiovascular and Thoracic Surgery. 2003; 2:193-195
-
Padro JM, Mesa JM, Silvestre J, Larrea JL, Caralps JM, Cerron F, Aris A. Subacute cardiac rupture: repair with a sutureless technique. Ann Thorac Surg. 1993;55:2023
-
Alejandro Aris. Surgical repair of left ventricular free wall rupture. Multimedia Manual of Cardiothoracics. 2004. doi:10.1510/mmcts.2004.
-
Malek G, Massas MD, Alexander SG. Surgical Repair of Mechanical Complications of Myocardial Infarction. World J Surg. 2004;28:847-856

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.