An atypical presentation of Neuroleptic Malignant Syndrome coexisting with Staphylococcus Pneumonia: a diagnostic challenge
Preaw Hanseree, Joanna M Tulczynska
Cite this article as: BJMP 2013;6(3):a620
|
|
Abstract Neuroleptic malignant syndrome (NMS) is a life-threatening neurologic disorder associated with the use of neuroleptic agents. NMS typically characterized by a distinctive clinical syndrome of mental status change, muscle rigidity, fever, and autonomic instability. Atypical cases may present without muscle rigidity and/or hyperthermia. Association of infection in atypical case can make the diagnosis challenging. We describe a case of NMS in a patient who presented with acute onset of altered mental status complicated with aspiration pneumonia. Keywords: neuroleptic malignant syndrome, atypical presentation, complication, pneumonia, infection |
Introduction
Neuroleptic malignant syndrome (NMS) is a life-threatening neurologic disorder associated with the use of neuroleptic agents. NMS is typically characterized by a distinctive clinical syndrome of mental status change, muscle rigidity, fever, and autonomic instability. Atypical cases may present without muscle rigidity and/or hyperthermia. Association of infection in an atypical case can make the diagnosis challenging. We describe a case of NMS in a patient who presented with acute onset of altered mental status complicated with aspiration pneumonia.
Case Report
A 22-year-old female with a history of schizophrenia and seizure disorder presented with acute onset of altered mental status. Her home medications included haloperidol, clonazepam, olanzapine, trazodone, topiramate, benztropine, and trihexyphenadyl. The patient was found unarousable by her mother. She had multiple suicidal attempts in the past (overdosed on acetaminophen, drank cleaning detergent, and cut her wrist). She usually medicated herself without supervision. On examination, the patient was drowsy, afebrile (Temp 36.8oC/98.3oF), hypotensive (BP 85/64 mmHg), tachycardic (HR 105 bpm), and tachypnic (24/min). She was noted to be grunting with both inspiratory and expiratory stridor; therefore she was intubated for airway protection. Initial drug screen was negative for all substances of abuse. Acetaminophen and salicylate levels were undetectable. Head CT was unremarkable. Supportive care was provided as the patient was suspected to be overdosed with multiple medications. On the second day of admission the patient developed fever of 38.9oC/102oF. Chest xray and chest CT showed bilateral infiltrations (Fig.1), so empirical piperacillin/tazobactam and vancomycin were started for aspiration pneumonia. Sputum culture came back positive for Methicillin-resistant Staphylococcus aureus. However, the patient remained febrile with a temperature of 39.6 oC /103.2oF, despite appropriate antibiotic treatment. We suspected that there might be some other coexisting condition causing high fever. Serum creatine kinase (CK) was checked and found to be 8,105 U/L, up from 106 U/L on admission. We considered the diagnosis of NMS based on alteration of mental status, hyperthermia, autonomic instability, and elevated CK level, with the use of neuroleptic agents, although the patient did not have any muscle rigidity. The patient was started on dantrolene in addition to intravenous fluid and antibiotics. Shortly afterwards temperature and CK level started to trend down (Fig.2,3). Dantrolene was subsequently increased to maximum weight-based dose. Her mental status was gradually improved and returned to baseline. She became afebrile on day 10 of dantrolene treatment and serum CK went back to normal level after 2 weeks. Then bromocriptine was started orally and continued for 2 weeks.

Figure 1A: chest xray on admission

Figure 1B: chest xray on second day of admission

Figure 1C: chest CT on second day of admission
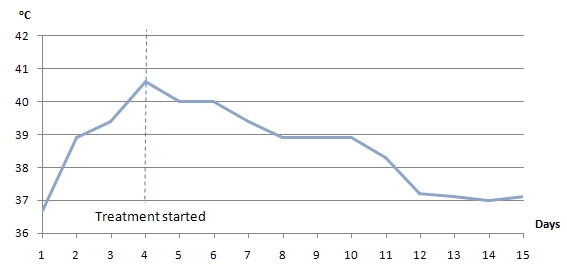
Figure 2. Temperature trend after starting treatment for NMS
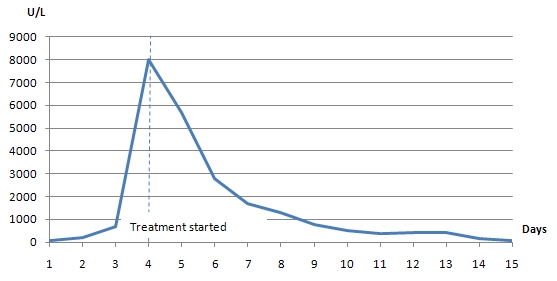
Figure 3. CK trend after starting treatment for NMS
Atypical presentations of NMS can sometimes be difficult to diagnose, as in our patient who presented with altered mental status, fever, and coexisting infection, in the absence of muscle rigidity. We emphasize the importance of a high index of suspicion of NMS in patients using neuroleptic agents.
Discussion
NMS is an idiosyncratic drug reaction to antipsychotic medications and a potentially life threatening condition that occurs in an estimated 0.07% to 2.2% of patients treated with antipsychotics.1 Patients typically present with fever, rigidity, changes in mental status, and autonomic instability, often attributed to first generation antipsychotics, in particular after the start of medication or an increase in dosage.2 Atypical cases of NMS without muscle rigidity and/or hyperthermia have been reported, usually associated with atypical antipsychotic treatment. It has been hypothesized that atypical cases represent early or impending NMS; however pathogenesis remains unclear.3 Risk factors that have been established in case series and case-control studies include agitation, dehydration, acute medical illness, concomitant use of other psychotropic drugs, intramuscular injections and high doses of antipsychotic medications.4-6
Complications of NMS are often consequences of its symptoms. Pneumonia is the most common complication found in 13% of patient with NMS, likely due to altered mental status combined with difficulty swallowing that lead to aspiration.7 Renal failure is the second most common complication (8%), as a result of rhabdomyolysis and myoglobinuria. Other complications have been reported including myocardial infarction, disseminated intravascular coagulation, deep venous thrombosis, pulmonary embolism, hepatic failure, sepsis, and seizure.8 Mortality rate of NMS was around 20-30%.9-10 With early identification and treatment, mortality has significantly reduced to averages 10%.6
Withdrawal of the causative agent is the first step in the management of NMS. Supportive therapy, in particular, hydration, fever reduction, and careful monitoring, is the mainstay of management of NMS. In mild cases, supportive treatment alone may be sufficient.4 Adding specific therapies, such as dantrolene, bromocriptine, and benzodiazepine to supportive measures has been shown to reduce time to complete recovery, from a mean of 15 days with supportive care alone, to 9 days with dantrolene, and 10 days with bromocriptine.1 In severe cases, empirical trial of specific pharmacological agents should be started promptly. Electroconvulsive therapy is found to be effective when pharmacotherapy has failed.11
Sometimes NMS is difficult to identify in the presence of critical illnesses which can obscure the manifestation of NMS. As in our case, the patient presented with altered mental status, fever, and autonomic instability which could be simply explained by the presence of pneumonia and sepsis. However, due to lack of clinical response after appropriate antibiotic treatment, other coexisting condition was suspected. It is important to have a high index of suspicion for NMS in the setting of antipsychotic therapy. An absence of muscle rigidity should not exclude a diagnosis of NMS when the rest of the clinical picture points to this diagnosis. Elevated CK level helps support the diagnosis of NMS in patients with atypical presentation. Discontinuation of offending agent and supportive care should initiate promptly, and specific pharmacotherapy should be considered in severe cases. An early diagnosis is the key to successful treatment and patient outcome.
Conclusion
NMS is a rare but potentially life-threatening condition. Atypical presentation makes it more difficult to identify in patients with critical illnesses. Aspirated pneumonia is one of the common complications of NMS and sometimes can obscure signs and symptoms of NMS and delay diagnosis. High index of suspicion for NMS in patients taking antipsychotics is crucial. If not recognized or left untreated, NMD may be fatal.
|
Competing Interests None declared Author Details PREAW HANSEREE, MD, Mount Sinai School of Medicine at Queens Hospital Center, New York, USA. JOANNA M TULCZYNSKA, MD, FCCP, Mount Sinai School of Medicine at Queens Hospital Center, New York, USA. CORRESPONDENCE: PREAW HANSEREE, Queens Hospital Center 82-68 164th Street, Jamaica, NY 11432, USA Email: phanseree@hotmail.com |
References
- Adnet P, Lestavel P, Krivosic-Horber R. Neuroleptic malignant syndrome. Br J Anaesth 2000;85(1):1290-1297
- Rosebush P, Stewart T. A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry 1989;146:717-25.
- Picard LS, Lindsay S, Strawn JR, Kaneria RM, Patel NC, Keck PE,Jr. Atypical neuroleptic malignant syndrome: diagnosis controversies and considerations. Pharmacotherapy 2008;28(4):530-535.
- Strawn JR, Keck PE, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry 2007;164:870-876
- Keck PE Jr, Pope HG Jr, Cohen BM, McElroy SL, Nierenberg AA: Risk factors for neuroleptic malignant syndrome. Arch Gen Psychiatry 1989;46:914-918
- Caroff SN, Mann SC: Neuroleptic malignant syndrome. Med Clin North Am 1993;77:185-202
- Addonizio G, Susman VL, Roth SD. Neuroleptic malignant syndrome: Review and analysis of 115 cases. Biol Psychiatry 1987;22:1004-1020
- Bilanakis N, Peritoqiannis V, Kalampokis G. Infections as complications of neuroleptic malignant syndrome. World J Biol Psychiatry 2009;10(4):973-976
- Robinson MB, Kennett RP, Harding AE, Legg NJ, Clarke B. Neuroleptic malignant syndrome associated with metoclopramide. J Neurol Neurosurg Psychiatry 1985;48:1304
- Saunders BP, Trewby PN. The neuroleptic malignant syndrome: a missed diagnosis? Br J Clin Pract 1993;47:170-171
- Trollor JN, Sachdev PS. Electroconvulsive treatment of neuroleptic malignant syndrome: a review and report of cases. Aust N Z J Psychiatry 1999;33(5):650-659

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




