Differential diagnosis of an abdomino-pelvic mass: Ganglioneuroma must be considered. A case history and literature review.
Mahmood Tariq, Khan Sadaqat Ali Professor, Sarwar Zeeshan, Rasool S Hamad, Anjum S Hasan and Tahir M Mohsin
Cite this article as: BJMP 2012;5(2):a519
|
|
Abstract An eleven year old female child presented with asymptomatic massive enlargement of the abdomen. It proved to be pelvic ganglioneuroma on complete surgical resection. Ganglioneuroma is a benign tumor of the sympathetic nervous system originating from the neural crest cells. Most common site is the posterior mediastinum. Pelvic ganglioneuroma is a rare entity and only a handful of cases have been published in the medical literature. |
Introduction:
Ganglioneuroma is a rare, benign, neuroblastic tumour that originates from the neural crest cells. Ganglioneuroma, ganglioneuroblastoma and neuroblastoma are three maturational manifestations of a common neoplasm in the progressive order of loss of differentiation. Ganglioneuromas may be found anywhere along the line of the embryonic neural crest, from clivus to sacrum and are very rare in the pelvis. Less than twenty cases have been described in the literature with various presentations based upon location including extradural, retroperitoneal, spinal, thoracic and one solely intradural medullary location. Ganglioneuromas may stay asymptomatic for a long period and give rise to no pressure symptoms either due to slow growth leading to progressive increase in size accompanied by adaptive changes. Ganglioneuromas demonstrate long-term disease-free survival even with an incomplete surgical removal. Here we present a case of a girl aged 11 years with pelvic ganglioneuroma.
Case Report:
A girl aged eleven years was brought from a remote hilly area in Pakistan by her mother to the city hospital many miles away. She had noticed that her daughter’s lower abdomen had progressively enlarged over last few months. Her menstrual cycle was normal so the mother was concerned that despite not being pregnant, her daughter had a distended abdomen as if she was pregnant She had a good appetite and unaltered bowel and bladder function. She had no heartburn, regurgitation, nausea, vomiting, heamatemesis or melaena. She denied any bleeding par rectum, shortness of breath, cough, loss of consciousness or convulsions. Her past medical history was mundane. She had not had any surgery in the past and was not taking any medication. Examination revealed a smooth, large, fixed hard mass in the right lower abdomen and pelvis. It was palpable in the pelvis on rectal examination which was otherwise normal. Liver or spleen was not palpable and she had no ascites. Her chest was clear, heart sounds were normal and there were no neurological abnormalities. Laboratory tests including FBC, LFT, U&E and Creatinine were normal. Her MRI scan was not of a good quality due to limitation of resources and technology at place of her diagnosis, but it showed an 11.4 x 11.8cm solid, well-defined mass arising from pelvis and extending up to the umbilicus. The mass showed intermediate low signals on T1 and hyper intense signals on T2 images (Fig. 1). Mid line surgical exploration was undertaken which showed a large, solid, retroperitoneal mass arising from sacral nerves within the pelvis. Mass was lying in front of great vessels, overlapping the confluence of common iliac vessels. The left ureter was displaced laterally while the right ureter was lying over the mass. The mass was excised completely. Post operative course was uneventful and patient was discharged home on the fifth post operative day.

Figure1: MRI showing showing a large soft tissue mass.
Macroscopically, the specimen was a 13x13x5cm rounded well-encapsulated mass (Fig. 2). Upon sectioning in vitro, mass was seen to be solid, whorled and grey white. Microscopically, groups and singly scattered ganglion cells were seen with surrounding neural tissue. There was no evidence of atypia, mitosis or necrosis. Features were suggestive of a ganglioneuroma. (Figure 3) The patient was well at two months follow up and required no further treatment.
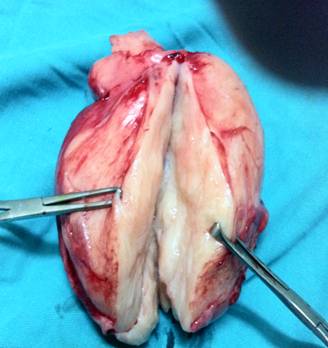
Figure2: Photograph of the resected specimen shows a well-encapsulated ovoid mass.
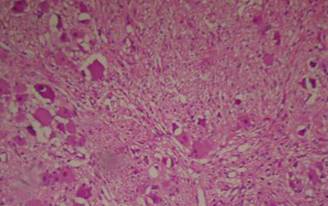
Figure 3 Microscopy showing scattered ganglion admist neuronal cells
Discussion:
Neuroblastoma, ganglioneuroblastoma and ganglioneuromas are tumours of sympathetic nervous system that arise from the neural crest cells.1 These tumours differ only in their progressive degree of cellular and extracellular maturity, with ganglioneuroma being the most mature hence well differentiated and neuroblastoma being the least.2 Ganglioneuroma are rare, benign and slow growing. They may occur spontaneously or as a down grading from therapy for Neuroblastoma with either chemotherapy or radiation.3 International Neuroblastoma Pathology Classification (INPC) has been devised after studying 552 such tumours. Out of 300 with favourable prognosis three groups were identified as; ganglioneuroma maturing (GN-M), ganglioneuroblastoma intermixed (GNB-I) and ganglioneuroblastoma nodular with favourable subset (GNB-N-FS). These are resectable in 91% cases in one or more surgical sessions. In contrast, the remaining 252 tumours had unfavourable prognosis and were called ganglioneuroblastoma nodular unfavourable subset (GNB-N-US). This group was not amenable to surgical resection and usually already had metastasis at the time of presentation.4
Ganglioneuromas although are mostly sporadic, may be associated with Neurofibromatosis (Von Recklinghausens Disease) and Multiple Endocrine Neoplasia type II (MEN).1 Ganglioneuroma usually presents before the second decade and rarely after the sixth.2 The median age at diagnosis has been reported to be approximately 7 years. There is a slight female preponderance.5 The common locations are the posterior mediastinum, and the retroperitoneal space. Retroperitoneal pelvic location is very rare and only few case histories have been reported.1
Although retroperitoneal ganglioneuromas are usually asymptomatic, some patients may get compression symptoms, diarrhea, hypertension, virilization and myasthenia gravis owing to release of certain peptides.1 Radiological examination may localize the lesion. MRI may show low intensity on T1-weighted images and heterogenous hyper intensity on T2-weighted images with gradual increasing enhancement on dynamic images.6
Surgical excision is sufficient for treatment of ganglioneuromas. Chemotherapy or radiotherapy has no role in the treatment. Even with an incomplete excision, close follow up alone may be adequate. If any progression of the tumour is seen then repeat laparotomy may be indicated.2
Conclusion:
Although pelvic ganglioneuroma is a very rare lesion, it should be considered in the differential diagnosis of any abdomeno-pelvic mass. As it is a slow growing tumour, gross total surgical removal with preservation of organ function is a feasible surgical option.
|
Competing Interests None declared Author Details MAHMOOD TARIQ, BSc, MBBS, LMSSA, MSc(Med Edu), MD, FRCP, Consultant Physician and Gastroenterologist, Ickenham, United Kingdom (Slides and all photographic material was provided by second author to the first author). SADAQAT ALI KHAN, MBBS, MCPS, FRCSEd, FICS, Head of Department, Surgical Unit III, Services Institute of Medical Sciences, Lahore. MUHAMMAD ZEESHAN SARWAR, MBBS, FCPS, Senior Registrar, Surgical Unit III, Services Institute of Medical Sciences, Lahore. SYED HAMAD RASOOL, MBBS, FCPS, Senior Registrar, Surgical Unit III, Services Institute of Medical Sciences, Lahore. SHAHID HASSAN ANJUM, MBBS, Medical Officer, Surgical Unit III, Services Institute of Medical Sciences, Lahore. MUHAMMAD MOHSIN TAHIR, MBBS, House Officer, Surgical Unit III, Services Institute of Medical Sciences, Lahore. CORRESPONDENCE: MAHMOOD TARIQ, Consultant Physician and Gastroenterologist, Ickenham, United Kingdom. Email: tm123@btinternet.com |
References
- Lamichhane N, Dhakal HP. Ganglioneuroma of pelvis – an unique presentation in a young man. Nepal Med Coll J 2006; 8: 288-91.
- Mounasamy V, Thacker MM, Humble S, Azouz ME, Pitcher JD, Scully SP, et al. Ganglioneuroma of the sacrum-a report of two cases with radiologic-pathologic correlation. Skeletal Radiol 2006; 35: 117-21.
- Hayes FA, Green AA, Rao BN. Clinical manifestations of ganglioneuroma. Cancer 1989; 63: 1211-4.
- Okamatsu C, London WB, Naranjo A et al. Clinopathological characteristics of ganglioneuroma and ganglioneuroblastoma: a report from CCG and COG. Paedr Blood Cancer, 2009 Oct; 53(4): 563-9
- Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, Berthold F. Metabolic activity and clinical features of primary ganglioneuromas. Cancer 2001; 91: 1905-13.
- Ichikawa T, Ohtomo K, Araki T, Fujimoto H, Nemoto K, Nanbu a, et al. Ganglioneuroma: Computed tomography and magnetic resonance features. Br J Radiol 1996; 69: 114-21

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




