Hamman’s syndrome in a parturient: a case report
Rajashree Chavan
Cite this article as: BJMP 2019;12(1):a007
|
|
Abstract Hamman’s syndrome is a potentially life threatening clinical condition characterised by peripartum subcutaneous emphysema and pneumomediastinum. This obstetric complication typically occurs in late pregnancy and labour and is frequently observed in young healthy primiparous women. I report a case postpartum pneumothorax and pneumomediastinum associated with spontaneous subcutaneous emphysema in primiparae. She presented to us in normal labour followed by Instrumental delivery under epidural anaesthesia. 10 hours post-delivery; she developed extensive subcutaneous emphysema, pneumothorax & pneumomediastinum with significant symptoms. She was successfully managed & discharged home after 24 hours of presentation of Hamman’s syndrome. Hamman’s syndrome is a rare obstetric complication which may present with/ without pneumothorax. Incidence is estimated at 1 in 100,000 deliveries. Approximately 200 such cases have been reported in literature worldwide. To my knowledge, this is one of the very few cases of Hamman’s syndrome with pneumothorax. Keywords: spontaneous pneumomediastinum, subcutaneous emphysema, pregnancy, labour |
Case Report:
A 33 year-old ASA1, primigravida, presented to our delivery suite with spontaneous onset of labour at 38 weeks of gestation. Epidural analgesia was commenced to alleviate her labour pains. Subsequently, she underwent an assisted vaginal delivery of a live male baby (weighing 4660 gms) using Keiland’s outlet forceps after 90 min second stage of labour. 10 hours postpartum, she complained of dyspnoea & severe central substernal chest pain. She was noted to have an unusual swelling of face and neck with oxygen saturations of 90 % on room air. Ascultation of chest revealed normal bronchovesicular breath sounds, normal heart sounds with absence of added sounds. Arterial blood gases showed an O2 tension of 11 kpa, CO2 tension of 5 kpa and pH of 7.34. The diagnosis of subcutaneous emphysema, pneumomediastinum and small left apical pneumothorax (Hamman’s syndrome) was confirmed on chest X-ray (CXR 1). We ruled out differential diagnosis of pulmonary embolism, Tension pneumothorax, angina pectoris, pericarditis, dissection of aortic aneurysm, mediastinitis, cardiac tamponade, chest infection & oesophageal tear. She was managed conservatively by close monitoring for complications, administration of supplemental oxygen and use of simple analgesics. She demonstrated a complete uneventful recovery over the next 24 hours with normalising of chest signs (CXR 2).
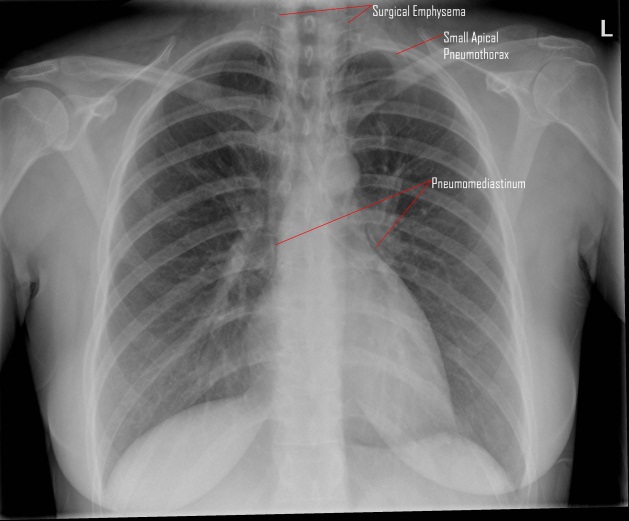
CXR 1: shows pneumomediastinum, extensive surgical emphysema & a left apical pneumothorax.
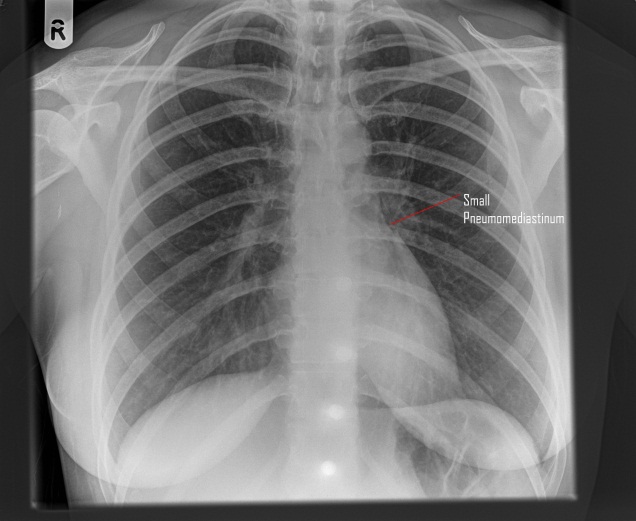
CXR 2: shows small pneumomediastinum, the surgical emphysema & pneumothorax resolved.
Discussion:
Hamman’s syndrome is named after Louis Hamman (1847-1946), the physician who first described it in 1945. The first reference to this condition was in 1618, when Louise Bourgeois, midwife to the Queen of France, wrote, “I saw that she tried to stop crying out and I implored her not to stop for the fear that her neck might swell”3.
Hamman’s syndrome usually occurs in the 2ndstage of labour & is associated with prolonged and protracted labour and larger than usual babies 4. However, the clinical presentation is often delayed to the postpartum phase as was clearly seen in our case. The condition seems to be provoked by any valsalva manoeuver such as vigorous coughing/vomiting/sneezing, forced physical activity & enormous efforts during spontaneous vaginal delivery. Its occurrence is usually related to the expulsive phase of labour when ‘pushing down’ actively raised the intraalveolar pressure. This may subsequently increase the intrathoracic pressure up to 50 mm of Hg or higher1. Rupture of marginal alveoli with air entering along the perivascular sheath into the mediastinum is the most likely mechanism, in our case. It is probable that, the air tracts through the fascial planes into subcutaneous and retroperitoneal tissues. Other reported mechanisms of Hamman’s syndrome include oesophageal rupture during childbirth, or pneumomediastinum related to asthmatic bronchospasm5 or chest infection, or dissection of pneumoperitoneum, secondary to epidural catheter placement or caesarean section1.
Palpable crepitus on face & neck is suggestive of subcutaneous emphysema & appearance of this emphysema in labour is the hallmark of pneumomediastinum. Other features of pneumomediastinum include substernal chest pain, dyspnoea, voice change, cough, sore throat and tachycardia1. Hamman’s sign, a fine auscultatory crepitation synchronous with the heartbeat, heard along the left sternal border; is sometimes observed in this condition2.
Chest X-ray and CT thorax are the diagnostic tests. Majority of the patients with Hamman’s syndrome have pneumomediastinum & subcutaneous emphysema without any pneumothorax and this requires supportive management with strict monitoring. Our patient demonstrated a small pneumothorax, which was managed conservatively. A surgical intervention in the form of subcutaneous air drainage may occasionally be indicated in severe cases.
Overall most cases have a benign, self-limiting course when the aggravating factors are no longer present. Published data indicates that subsequent pregnancies pose no additional risk of recurrence5.
Conclusion:
Since Hamman’s syndrome is a potentially dangerous complication of normal childbirth. We propose that every obstetric anaesthetist and obstetrician should be aware of this syndrome.
|
Competing Interests None declared Author Details RAJASHREE CHAVAN, M.B.B.S D.A M.D Anaesthesiology F.R.C.A, Consultant Anaesthetist Basildon & Thurrock University Hospital NHS Foundation Trust, United Kingdom. CORRESPONDENCE: RAJASHREE CHAVAN, Consultant Anaesthetist, Basildon & Thurrock University Hospital NHS Foundation Trust, Nethermayne, Basildon, Essex, SS16 5NL, United Kingdom. Email: vidula77@doctors.net.uk |
References
- Spontaneous pneumomediastinum in 3rd trimester of pregnancy-Discussion. Ann ThoracicCardiovascular Surg 2006
- Intrapartum pneumomediastinum associated with subcut emphysema. Canadian Medical Association Journal 1998
- Subcutaneous emphysema in labour. Anaesthesia 1993; 48:139-140
- Pleural disease in pregnancy. Clinical Chest Medicine 1992; 13:667-78
- Mediastinal & subcutaneous emphysema in pregnant patient with asthma. BJOA 1980; 87:440-3

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




