Improving Communication Skills Using Simulation Training
Priya Subramanian and Krishanthi Sathanandan
Cite this article as: BJMP 2016;9(2):a911
|
|
Abstract Introduction Medical trainees are required to manage complex communication scenarios effectively on entering specialty training. Whilst significant emphasis is placed on undergraduate basic communication skills training, there is little formal postgraduate training. Communicating effectively with patients and families plays a vital role in providing high quality care, and a significant proportion (10.5% in 2012/2013) of medical complaints pertain to poor communication.(1) We conducted a survey of junior medical trainees. This showed only 50% felt somewhat competent in engaging in difficult communication scenarios, while 88% experienced significant challenges. All expressed interest in further training. Methods Simulation-based training is known to provide a controlled environment in which it is safe to learn from errors (2), and improves learner outcomes. (3) We created a course using simulation to develop medical trainees’ competencies in advanced communication skills. Two sessions were conducted. Professional actors and role-play exercises were used, with interactive feedback from a senior doctor in elderly/palliative care medicine. Scenarios concentrated on end of life discussions and capacity assessment. Results Feedback was obtained from participants using a Likert scale of 1 – 5. 100% felt the content was useful, and their skills and confidence had increased. All trainees and facilitators felt this would be beneficial for others. Discussion The European Working Time Directive has led to difficulty gaining proficiency in key skill areas due to reduced patient encounters. Simulation training is now routinely used to tutor trainees. This pilot programme shows the value of using this modality to teach higher-level communication skills. |
Introduction
Communicating effectively with patients and families is a vital component of high quality care. Studies have shown that patients feel excellent communication in consultations is vital for instilling confidence in the medical practitioner.1,2 There is evidence that doctors are not meeting this fundamental need.3
Some consider it an ethical obligation of doctors to balance their training needs against providing optimal care for patients. It is well known that junior trainees have significant level of performance anxiety that translates through to their consultations.4
Simulation based training is now an integral part of postgraduate curriculum in training a variety of medical specialties in managing acute scenarios. As an education method it provides a controlled environment in which it is safe to learn from errors,5 and improves learner outcomes.6 Simulation has been shown to be a valid approximation of true clinical practice.7 It therefore allows trainees to reach higher levels of proficiency prior to embarking on real patient encounters.
Current Core Medical Trainees (i.e. junior doctors who have embarked on the first stage of physician training within England) in the London deanery are expected to be able to manage complex communication scenarios effectively prior to entering specialty training. This is demonstrated by requirements set out in the Core Medical Curriculum, as detailed in Box 1. Whilst significant emphasis is placed on communication skills training in basic scenarios at a medical student level, there is very little formal postgraduate communication skills training within this deanery and others.
Box 1: Excerpts from Core Medical Trainee curriculum
| Counsel patients, family, carers and advocates tactfully and effectively when making decisions about resuscitation status, and withholding or withdrawing treatment
Able to explain complex treatments meaningfully in layman's terms and thereby to obtain appropriate consent even when there are problems of communication and capacity Skillfully delivers bad news in any circumstance including adverse events |
This deficit in training led us to conduct a survey exploring Core Trainees’ views regarding communication skills training in the London deanery. Findings from the survey are detailed in Box 2.
Box 2: Results from Core Trainee Survey
| 83% received less than 2 hours of post-graduate training in communication skills since the start of Core Medical Training
Only 50% felt somewhat competent in engaging in difficult communication scenarios 88% reported significant challenges when conducting these discussions. They have had difficult on-calls experiences relating to communication difficulties 100% displayed interest in attending further Simulation Training in advanced communication skills |
Method
We devised a pilot project using simulation to develop trainees’ competencies in advanced communication skills. After application to our local training board, we secured funding to run a number of sessions for core medical trainees within the London area.
The objectives of our pilot project were to provide experience of realistic communication based scenarios in a structured and safe environment to core trainees; provide feedback on trainees’ communication styles and offer suggestions for improvement; improve confidence of trainees in difficult communication situations.
Each session was conducted in an afternoon session and candidates were divided into three groups of three trainees who would remain together for the entire session. We ran four sessions, with a total of 36 trainees. Each group was facilitated by a consultant or a higher trainee in either elderly or palliative care medicine, given our focus on resuscitation/end of life discussions and assessment of capacity. We employed three actors to rotate around each group performing a variety of roles including patients and relatives. With a total of six scenarios, each trainee had the opportunity to participate in at least two scenarios lasting approximately 15 minutes, with feedback thereafter for approximately 10 minutes.
The scenarios employed were based on personal experience of regularly occurring, challenging communication situations encountered in our own clinical practice. We created detailed scripts for the actors as well as corresponding clinical vignettes for the candidates.
The scenarios were:
- End-of-life discussion with a challenging family regarding a patient with end-stage dementia.
- Discussing resuscitation with a family opposed to do not attempt resuscitation (DNAR) regarding an acutely unwell patient with poor functional baseline.
- Discussing resuscitation with a young patient with metastatic cancer undergoing palliative chemotherapy who has little understanding of the terminal nature of the disease.
- Assessing mental capacity regarding discharge planning in a patient with mild to moderate dementia.
- Assessing mental capacity regarding treatment in a patient with moderate learning difficulties.
- Assessing mental capacity in a medically unwell patient with mental health issues who wishes to self discharge from the ward.
Box 3 outlines the session structure.
Box 3: Timetable for the session
| 12.30-12.45: | Actors briefing |
| 12.45- 13.00: | Facilitators briefing |
| 13.00-13.30: | Core trainee briefing |
| 13.30-14.45: | Scenarios 1-3 in small groups |
| 14.45-15.00: | Tea/Coffee break |
| 15.00-16.15: | Scenarios 4-6 in small groups |
| 16.15-16.45: | Feedback and closing |
Results
Written feedback was obtained from all participants by distributing a post-course evaluation form, with a 100% response rate. A number of areas were assessed via a Likert scale of 1 – 5, with 1 being ‘not at all’ and 5 being ‘very much’. 100% of trainees felt the content was useful and their knowledge/skills had increased. 100% felt more confident after the session and all trainees and facilitators felt this would be beneficial for medical trainees. A full breakdown of results is detailed in Table 1.
Table 1: Results from post-course feedback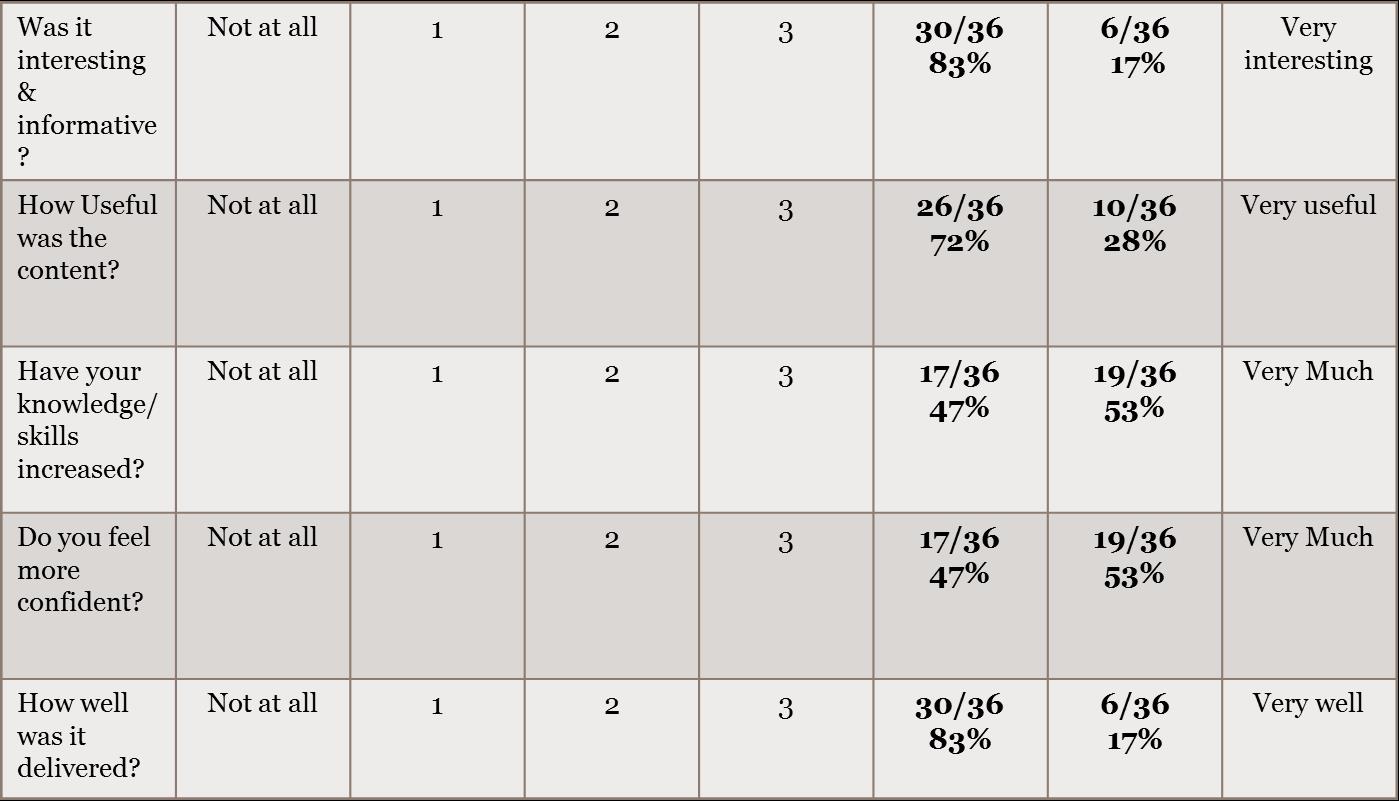
The post-course feedback form allowed for free text feedback from participants, with some individual examples given below:
“Realistic scenarios - good opportunity to experience them and get feedback in a safe environment, good practice of common communication problems”
“It builds confidence in dealing with these situations and provides basis for building up ”
“This work dealt with complicated cases and actors were not too easy which I liked. Good and unforgettable”
Discussion
With the European Working Timing Directive and resulting shorter working hours, gaining proficiency in a number of key skill areas is limited due to reduced patient encounters. A recurrent complaint among core medical trainees is the lack of observed clinical encounters that leads to individualised feedback.
Feedback from more experienced speciality practitioners was only one component of our attendees learning experience. They also benefited from personal practise in a non-threatening environment, observation of their colleagues communication styles and finally learning through reflection with their colleagues
This innovation has shown a clear benefit in amplifying the confidence and preparedness of our core medical trainees in approaching these higher level communication scenarios. Future directions include introducing quantitative assessments pre- and post- course to objectively demonstrate improved confidence and performance. Providing the course to trainees in other specialties as well as across the multidisciplinary team would also be beneficial given the universal requirement of healthcare professionals to communicate skilfully.
|
Competing Interests None declared Author Details PRIYA SUBRAMANIAN, MBBS BSC, University College London Hospital, 235 Euston Rd, London, NW1 2BU, England. KRISHANTHI SATHANANDAN MBBS BSC, University College London Hospital, 235 Euston Rd, London, NW1 2BU, England. CORRESPONDENCE: PRIYA SUBRAMANIAN, MBBS BSC, University College London Hospital, 235 Euston Rd, London, NW1 2BU, England. Email: psubramanian@doctors.org.uk |
References
- Jackson JL . Communication about symptoms in primary care: impact on patient outcomes. Journal of Alternative and Complement Medicine. 2005;11 Suppl 1:S51-6.
- Hagerty RG1, Butow PN, Ellis PM, Lobb EA, Pendlebury SC, Leighl N, MacLeod C, Tattersall MH. Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis. Journal of Clinical Oncology. 2005 Feb 20;23(6):1278-88.
- Kissane DW1, Bylund CL, Banerjee SC, Bialer PA, Levin TT, Maloney EK, D'Agostino TA. Communication skills training for oncology professionals. Journal of Clinical Oncology. 2012 Apr 10;30(11):1242-7. doi: 10.1200/JCO.2011.39.6184. Epub 2012 Mar 12.
- Ziv A1, Wolpe PR, Small SD, Glick S. Simulation-based medical education: an ethical imperative. Academic Medicine. 2003 Aug;78(8):783-8.
- Maran NJ, Glavin RJ. Low- to high-fidelity simulation - a continuum of medical education? Medical Education. 2003 Nov;37 Suppl 1:22-8.
- McGaghie WC1, Issenberg SB, Petrusa ER, Scalese RJ. Effect of practice on standardised learning outcomes in simulation-based medical education. Medical Education. 2006 Aug;40(8):792-7.
- Issenberg SB1, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Medical Teacher. 2005 Jan;27(1):10-28.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




