Postural Orthostatic Tachycardia Syndrome (POTS): Evaluation and Management
Ronald Conner, Mujeeb Sheikh and Blair Grubb
Cite this article as: BJMP 2012;5(4):a540
|
| Abbreviations: JHS - Joint hypermobility syndrome, POTS - Postural Orthostatic Tachycardia Syndrome, SSRI - serotonin reuptake inhibitor, SNRI - norepinephrine reuptake inhibitor, EPO - erythropoietin |
Case Presentation
A 29 year-old woman had been well until 7 months previously when, after a viral syndrome, she developed palpitations, fatigue, and frequent episodes of light headedness and near syncope. On further questioning she notes exercise intolerance and dyspnea on exertion. She has stopped working as cashier. Her mother thinks she is having panic attacks and needs “something to calm her nerves.” ECG, echocardiogram, and endocrine evaluation are all normal. On physical examination, she displayed a postural heart rate increase of 35 beats per minute on standing, along with a 15mmHg fall in diastolic blood pressure.
Introduction
Disorders of the autonomic nervous system present unique challenges to the practicing clinician. These syndromes have a significant impact on quality of life, offer subtle diagnostic clues, and have a propensity to mimic other disease processes. For these reasons clinicians should have basic familiarity with the differentiating features of autonomic disorders. While much investigation has focused on Neurocardiogenic syncope, a distinct subgroup has emerged characterized by postural tachycardia and exercise intolerance. Postural orthostatic tachycardia syndrome (POTS) is the final common pathway of a heterogeneous group of underlying disorders that display similar clinical characteristics .1
The constellation of symptoms associated with POTS reflects underlying dysautonomia including palpitations, exercise intolerance, fatigue, lightheadedness, tremor, headache, nausea, near syncope, and syncope. Foremost amongst these is orthostatic intolerance. Besides being limited in the functional activities of daily living, increased sleep disturbances including excess daytime sleepiness, fatigue are also common and have been associated poor health-related quality of life. 2 We aim to discuss the clinical presentation, classification, evaluation and management of POTS.
Diagnosis
The current diagnostic criteria for POTS is the presence of orthostatic intolerance symptoms associated with a sustained heart rate increase of 30 beat per minute (bpm) or absolute rate exceeding 120 bpm within the first 10 minutes of standing or upright tilt in the absence of other chronic debilitating disorders, prolonged bed rest, or medications that impair vascular or autonomic tone. 3 Most patients will have orthostatic symptoms in the absence of orthostatic hypotension (a fall in BP >20/10 mmHg). A grading system for POTS has been developed (Table 1). This system focuses on the functional severity of orthostatic intolerance in a way similar to the NYHA heart classification.
The physical exam should be methodical and directed. Supine, sitting, and immediate standing heart rate and blood pressure should be recorded. Orthostatic tachycardia and acrocyanosis of the lower extremities may be the only physical signs in these patients. Standing and supine blood pressure measurements and baseline electrocardiogram are generally recommended. In patients with physical examination or clinical history suggestive of cardiovascular abnormalities, other diagnostic test including echocardiogram , stress test or coronary angiography may be indicated before a tilt test. In addition, other possible clinical disorders with similar clinical manifestations must be kept in mind and ruled out. Upright tilt test remains the diagnostic test of choice for POTS and other autonomic disorders. Implantable loop recorders, electrophysiological tests and Holter monitoring are not helpful in the evaluation of these disorders. Supine and upright serum catecholamine levels should be obtained if hyperadrenergic type is suspected. In the presence of gastrointestinal symptoms bowel motility studies may reflect the degree of involvement and help to tailor therapy. 4
| Table 1 : The Grading of Orthostatic Intolerance* |
| Grade 0 Normal orthostatic tolerance |
| Grade 1 Orthostatic symptoms are infrequent or occur only under conditions of increased orthostatic stress Subject is able to stand >15 minutes on most occasions Subject typically has unrestricted activities of daily living |
| Grade II Orthostatic symptoms are frequent, developing at least once a week Orthostatic symptoms commonly develop with orthostatic stress Subject is able to stand >5 minutes on most occasions Some limitation in activities of daily living is typical |
| Grade III Orthostatic symptoms develop on most occasions and are regularly unmasked by orthostatic stresses Subject is able to stand for >1 minute on most occasions Patient is seriously incapacitated, being bed or wheelchair bound because of orthostatic intolerance Syncope / presyncope is common if patient attempts to stand |
| *Symptoms may vary with time and state of hydration and circumstances. Orthostatic stresses include prolonged standing, a meal, exertion, and head stress. |
Classification and Clinical Features
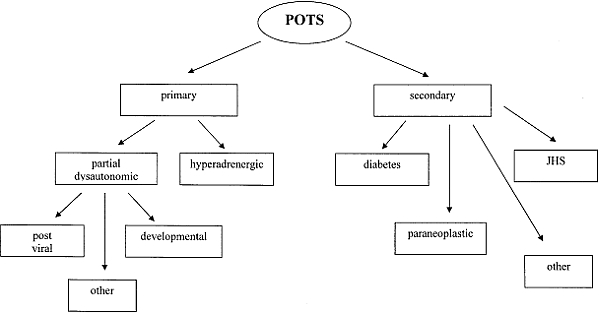
POTS is a heterogeneous group of disorders resulting in a common clinical scenario. This syndrome is classified as being either primary or secondary. Primary POTS is idiopathic and not associated with other disease processes. Secondary POTS occurs in association with a known disease or disorder. Subtype classification affects management and is therefore essential.1,4 (Figure 1)
Partial dysautonomic (PD) POTS (also referred to as Neuropathic POTS) is the predominant form.1, 2 This is a mild peripheral autonomic neuropathy, characterized by inadequate peripheral vasculature constriction in the face of orthostatic challenge. Female predominance is seen with 5:1 female to male ratio. Presentation is commonly abrupt onset of symptoms after a febrile viral illness, pregnancy, immunization, sepsis, surgery, or trauma. The etiology of PD type POTS is postulated to be an autoimmune molecular antigen mimicry type pathogenesis. Serum autoantibodies to peripheral autonomic ganglion alpha-3 acetylcholine receptors may be positive in 10-15% of the cases. Anhidrosis of lower extremities is seen in more than 50% of these patients at quantitative sudomotor axon reflex testingDependent blood pooling when upright is greater than normal and heart rate and contractility increase as normal compensatory physiologic mechanisms to maintain cerebral perfusion. This autoregulatory response may initially be fully compensatory; however, peripheral venous pooling may increase with time and exceed this compensatory effect. Patients with PD type POTS become dependent on the skeletal muscle pump to augment their autoregulatory physiology. Ultimately, venous blood pooling increases beyond the body’s total ability to compensate and adequate blood pressure maintenance fails.
“Developmental” partial dysautonomic POTS is an adolescent subtype.6 The mean age of onset is 14 years. The clinical scenario is that of orthostatic intolerance following a period of very rapid growth. Symptoms are progressive and peak at a mean age of 16 years. Orthostatic intolerance may be severe, including severe headaches, and can be functionally disabling. Following their peak symptoms will slowly improve and resolve into young adulthood (19-24 years). Roughly 80% of patients with developmental PD POTS will experience complete resolution of symptoms. The etiology of this subtype is unclear and appears to be a transient period of autonomic imbalance occurring in rapidly growing adolescents.
Hyperadrenergic POTS is less common than the PD type ,7This form is characterized by a gradual onset with slowly progressive symptoms. Patients report experiencing tremor, anxiety, and cold clammy extremities with upright posture. 7 Many patients note increased urine output when upright. True migraine headaches may be seen in over half of patients.7 Gastrointestinal symptoms in the form of recurrent diarrhea were seen in 30% of the patients. In contrast to PD type of POTS, the hyperadrenergic form demonstrates elevated serum catecholamine levels with serum norepinephrine levels >600ng/ml. This may be a familial syndrome in some instances determined by a careful history. The etiology of hyperadrenergic POTS is felt to be genetic with a single point mutation resulting in a dysfunctional norepinephrine reuptake transporter protein present in the intrasynaptic cleft. The result is excessive norepinephrine serum spillover with sympathetic stimulation resulting in a relative hyperadrenergic state appearing similar to pheochromocytoma. 8
A connective tissue disorder has been an increasingly recognized etiology of secondary POTS 9 . Joint hypermobility syndrome (JHS) is an inherited condition characterized by joint hypermobility, connective tissue fragility, and soft velvety skin with variable hyperextensibility. The condition is associated with ecchymotic predisposition, premature varicose veins, diffuse muscle and joint pain, and orthostatic acrocyanosis. The etiology of POTS in JHS patients is thought to be due to abnormal vascular (venous) elastic connective tissue. During orthostatic stress and increased hydrostatic pressure these patients exhibit increased vessel distensibility and orthostatic intolerance. Excessive peripheral venous pooling and compensatory tachycardia follows. Up to 70% of JHS patients suffer from some degree of orthostatic intolerance. It is observed that adolescent PD POTS patients have features similar to JHS patients and further studies may determine the significance of this potential relationship 10.
Secondary POTS refers to a group of conditions which result in peripheral autonomic denervation with sparing of cardiac innervation. Most commonly, secondary POTS is associated with diabetes mellitus. Less commonly, this form may occur with heavy metal intoxication, multiple sclerosis, parkinsonism and chemotherapy, especially vinca alkaloids.11,12
Severe autonomic nervous system disorders may present as POTS. These may include pure autonomic failure or multiple system atrophy. Paraneoplastic syndrome associated with adenocarcinoma of the lung, breast, ovary, or pancreas may also present as POTS. These tumors produce auto-antibodies targeting the acetylcholine receptors in the autonomic ganglia in a manner similar to post-viral syndromes.
Figure 1. Subtypes of postural orthostatic tachycardia syndrome
Evaluation and Management
Treatment is generally individualized to each patient. Confounding pharmacology should be identified and stopped if possible (Table 2). The presence of secondary POTS should be considered. Underlying diagnoses causing or augmenting POTS should be identified and treated appropriately. Deconditioning is frequent seen in POTS patient and a deliberate aerobic reconditioning program should be a component of the treatment plan. 13 This is encouraged to begin promptly working up to a goal of 20-30 minutes of activity at least 3 times a week. Resistance training of the lower extremities is helpful to increase the efficacy of the skeletal muscle pump. Salt and water ingestion are the most common employed non-pharmacolgical therapeutic intervention for POTS. Although, the intravenous saline infusion has been associated with reduction in standing tachycardia, the effect on this intervention on the symptom reduction remains unknown 14 . In general, since low blood volume may exacerbate symptoms patients are encouraged to have liberal salt and water intake. Excluding hyperadrenergic POTS, daily fluid and sodium intake should be greater than 2 liters and 3-5 grams.
| Table 2: Pharmacologic Agents That May Cause or Worsen Orthostatic Intolerance | |
| Angiotensin-converting enzyme inhibitors Alpha receptor blockers Calcium channel blockers Beta blockers Phenothiazines Tricyclic antidepressants Bromocriptine Ethanol |
Opiates Diuretics Hydralazine Ganglionic-blocking agents Nitrates Sildenafil citrate Monoamine oxidase (MAO) inhibitors |
The goal of pharmacotherapy in the treatment of POTS is to ameliorate the symptoms of POTS and thus maintain the functional capacity. Currently no drug is US FDA approved for the treatment of POTS. All pharmacology is inherently off-label. (Table 3).
| Table 3: Therapeutic Options in POTS | |||
| Treatment | Application | Form Effective in | Problems |
| Reconditioning | Aerobic exercise 20 min 3 times / week | PD, H | If too vigorous may worsen symptoms |
| Hydration | 2 liters PO/day | PD | Edema |
| Salt | 2-4 grams/day | PD | Edema |
| Fludrocortisone | 0.1-0.2 mg PO daily | PD | Hypokalemia, hypomagnesemia, edema |
| Midodrine | 5-10 mg PO TID | PD | Nausea, scalp pruritus, supine hypertension |
| Methylphenidate | 5-10 mg PO TID | PD | Anorexia, insomnia, dependency |
| Bupropion | 150-300 mg XL daily | PD, H | Tremor, agitation, insomnia |
| SSRI-Escitalopram | 10 mg PO Daily | PD, H | Tremor, agitation, sexual problems |
| Pyridostigmine | 30-60 mg PO BID | PD | Nausea, diarrhea |
| Erythropoietin | 10,000-20,000 IV SQ weekly | PD | Pain at injection site, expensive |
| Octreotide | 50-200 ug SQ TID | PD | Nausea, diarrhea, gallstones |
| Clonidine | 0.1-0.3 mg PO BID; 0.1-03 mg patch weekly | H | Dry mouth, blurred vision |
| Labetalol | 100-200 mg PO BID | H | Fatigue |
| PD = partial dysautonomic; H = hyperadrenergic; POTS = postural tachycardia syndrome | |||
Majority of the evidence for the use of different pharmacological agents in the management of POTS is based on some small randomised , observational and retrospective single center studies. In clinical practice most patients are treated with a single agent and second medication from different class with a different mechanism of action is added in case of treatment failure. Resistant cases are often treated with polypharmacy.
Fludrocortisone, a potent mineralocorticoid resulting in sodium retention, augmented fluid volume, and sensitized peripheral alpha adrenergic receptors. The effects are more pronounced in the younger population. Starting dose is 0.1-0.2 mg daily with a maximum dose of 0.4 mg. Common side effects include electrolyte imbalance and hypertension. In a study of 11 female POTS patients, fludricortisone alone or in combination with bisoprolol was associated with improvement in symptoms 15. Midodrine is an alpha -1 adrenoreceptor agonist and causes both arterial and venous vasoconstriction. It is commonly used as add on therapy and with starting dose at 5 mg orally three times a day. In our clinical experience we advise patients to take their first dose of midodrine 15 minutes prior to getting out of bed. An additional 5mg dose can be used for breakthrough symptoms. Midodrine is usually well tolerated with the most common complaints being nausea, “goose bumps,” and scalp pruritus. In a small study of 6 patients with POTS acute combination therapy of midodrine (10mg) with octreotide (0.9mcg/kg) was significantly associated with reduction in upright tachycardia and improved standing time.In another study of 53 children with POTS, midodrine was significantly associated with both higher clinical cure rate and reduced recurrence rate as compared to children treated with metoprolol or conventional therapy.
Patients may continue to be symptomatic despite dual-therapy as outlined above. In this population we add a serotonin reuptake inhibitor (SSRI) or norepinephrine reuptake inhibitor (SNRI). SSRI therapy has been found to be helpful in the prevention of neurocardiogenic syncope. However, SNRI therapy is more useful in the treatment of POTS. Usually, we use bupropion XL beginning with 150 mg orally daily titratable to 300 mg daily if necessary.
The most effective SSRI therapies combine serotonin and norepinephrine reuptake inhibition (venlafaxine and duloxetine). The agents are usually well tolerated with the most common side effects being gastrointestinal upset, tremor, sleep disturbance, and less commonly agitation and sexual dysfunction. Bupropion and SSRI therapy can be combined to achieve a similar effect.
Pyridostigmine is an acetylcholinesterase inhibitor that facilitates sympathetic and parasympathetic ganglionic neural transmission. In our single center experience of 203 patients of POTS treated with pyridostigmine; improved symptoms of orthostatic intolerance were seen in 88 of 203 (43%) of total patients or 88 of 172 (51%) who were able to tolerate the drug. Fatigue (55%), palpitations (60%), presyncope (60%), and syncope (48%) were the most common symptoms that improved with pyridostigmine. Further, symptom reduction correlated with a statistically significant improvement in upright HR and diastolic blood pressure after treatment with pyridostigmine as compared to their baseline hemodynamic parameters (standing HR 94 ± 19 vs 82 ± 16, P < 0.003, standing diastolic blood pressure 71 ± 11 vs 74 ± 12, P < 0.02). Gastrointestinal problems were the most common adverse effects (n = 39, 19%) seen in our study. 18
Severely affected and refractory patients may benefit from erythropoietin (EPO) therapy. EPO increases red cell mass, central blood volume and augments response of blood vessels to the angiotensin-II and thus causes vasoconstriction. These effects are quite useful in the treatment of orthostatic disorders. Prior to initiation of EPO therapy obtain a complete blood count (CBC), total iron binding capacity, serum iron and ferritin levels. Hematocrit (HCT) levels must be monitored and should remain less than 50 on EPO. The starting dose is 10,000 units via subcutaneous injection once weekly. There is a 4-6 week delay between a given dose and the full clinical effect. The hematogenic and hemodynamic affects are independent but may occur simultaneously. A goal HCT of low to mid 40 will often result in optimum hemodynamic augmentation. Monitoring during EPO therapy should include monthly CBC to document HCT less than 50. EPO therapy may infrequently result in a “serum sickness” type reaction characterized by nausea, fever, chills, and general malaise. In another study of 39 patients (age 33 ± 12, 37 females) with resistant form of POTS, we reported sustained improvement in twenty-seven (71%) patients at mean follow-up of six month with EPO therapy. Eighty (21%) failed to respond to therapy while as 3 (8%) improved with therapy at 3months. Also, erythropoietin significantly improved sitting diastolic blood pressure but had no effect on other hemodynamic parameters.19 We reserve EPO therapy for patients that are refractory or intolerant of other forms of treatment because of its considerable expense and subcutaneous route of administration.
Beta blocker therapy such as metoprolol tartrate may be beneficial in adolescent type POTS patients. In a single center retrospective study of 121 patients with possible POTS, written survey at follow-up were used to evaluate response to therapy with beta-blockers and midodrine. 47 adolescents responded to survey (Walker Functional Disability Inventory Survey) and reported improvement with a β-blocker (100% vs 62%, P = 0.016) and more attributed their progress to medication (63.6% vs 36.4%, P = 0.011) than did those treated with midodrine 20 .In addition, beta-blocker therapy was associated with improved quality of life. Great caution should be taken in using beta-blocker therapy in a rare form of hyperadrenergic POTS secondary to the mast cell activation disorders. Octreotide is a somatostatin analogue with potent vasoconstrictive effects and is useful in the treatment of orthostatic disorders. In patients with resistant POTS, octreotide may be a useful as add on therapy. It is administered by subcutaneous injection 2-3 times daily. The stating dose is 50 ug and may be titrated up to 100-200 ug three times daily.
Agents that block the release or effect of norepinephrine (noradrenaline) are very effective for hyperadrenergic type POTS patients. We use clonidine starting at 0.1 mg orally twice daily and titrating up as needed. The patch form may be preferable to some patients and has the added benefit of providing a steady state drug release for one week. Labetalol, an alpha and beta receptor blocker, is also useful in this group of patients. Dosages of 100-400 mg orally twice daily are used. Methyldopa may have a role in highly selected patients with POTS. Symptom control may be improved with both the SSRI and SNRI classes of medications.
Inappropriate sinus tachycardia (IST) is an important confounding finding in suspected POTS patients. This syndrome is similar to hyperadrenergic type POTS. The clinical presentation may be similar with IST being more common in females. These disease states display and exaggerated response to isoproterenol infusion. It has been postulated that they may represent different states of the same pathologic process. A greater degree of orthostatic change in heart rate is seen in POTS patients. The supine rate rarely exceeds 100 bmp (IST will often be >100). Postural changes in serum norepinephrine levels are much more pronounced in POTS patients. It is important to differentiate POTS and IST. Radiofrequency ablation of the sinus node will rarely benefit hyperadrenergic POTS patients and will make PD POTS patients markedly worse.
Treatment of secondary POTS should focus primarily on the underlying disorder to the greatest extent possible. Diabetes mellitus or JHS related POTS are treated as PD POTS. Secondary POTS due to sarcoidosis or amyloidosis may benefit from steroid therapy. Secondary POTS that is paraneoplastic may completely resolve with treatment of the underlying malignancy but may also respond to pyridostigmine.
Patients suffering from POTS have a disease that affects many aspects of their life. They are often unable to take advantage of meaningful employment or education opportunities. The pervasive life change experienced often results in significant psychosocial disruption as they may be excluded from social norms and certain environments. Frequently, patients require psychologists, social workers, and lawyers to address these aspects of living with POTS. The treating physician is a prominent and central figure who is a beacon of hope for this population. A positive, caring, and nurturing attitude may be the best medicine and lead to a rewarding rapport where an otherwise challenging disease exists.
Prognosis
There is limited data on the prognosis of POTS patients. Recent short term follow-up studies have shown better prognosis in patients with POTS. 21 Roughly 50% of post-viral POTS patients make a meaningful recovery over about 2-5 years. Meaningful recovery may be defined as the absence of orthostatic symptoms and the ability to perform the activities of daily living with little or no restriction. Some patients experience a partial recovery and still others may demonstrate a progressive functional decline with time. As a general principle, a younger age of onset portends a better prognosis. A majority of patients tend to adopt different lifestyle modifications including increased fluid and salt intake to improve and reduce exacerbation of the POTS symptoms. In secondary POTS syndromes have a prognosis consistent with the underlying causative disorder.
Conclusion
Disruption of normal autonomic function may manifest as one of a heterogeneous group of clinical disorders collectively referred to as postural orthostatic tachycardia syndrome. Treatment is most successful when diligence has been taken to investigate the underlying disorder or POTS subtype and a comprehensive targeted treatment program is instituted with frequent follow up. Goals of care should focus on functional milestones and maintenance of function.
|
Competing Interests None declared Author Details RONALD CONNER, MD, Cardiovascular fellow, Cardiovascular division, Department of Internal Medicine, University of Toledo Medical Center, USA. MUJEEB SHEIKH, MD, Cardiovascular fellow, Cardiovascular division, Department of Internal Medicine, University of Toledo Medical Center, USA. BLAIR GRUBB, MD, Professor of Medicine, Cardiovascular division, Department of Internal Medicine, University of Toledo Medical Center, USA. CORRESPONDENCE: Mujeeb Sheikh, MD, Cardiovascular fellow, Cardiovascular division, Department of Internal Medicine, University of Toledo Medical Center, 3000 Arlington Avenue, Toledo, Ohio, USA, 43614. Email: Mujeeb.sheikh@utoledo.edu |
References
- Kanjwal Y, Kosinski D, Grubb BP: The postural tachycardia syndrome: Definition, diagnosis and management. Pacing Clin Electrophyiol 2003;26:1747-1757.
- Bagai K, Song Y, Ling JF et al.Sleep disturbances and diminished quality of life in postural tachycardia syndrome. J Clin Sleep Med. 2011 Apr 15; 7(2):204-10.
- Grubb BP, Kanjwal Y, Kosinski DJ: The Postural Tachycardia Syndrome: A Concise Guide to Diagnosis and Management. J Cardiovasc Electrophysiol 2006;17:108-112.
- Grubb BP: Postural Tachycardia Syndrome. Circulation 2008;117:2814-2817
- Thieben MJ, Sandroni P, Sletten DM, et al. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin Proc. 2007 Mar; 82(3):308-13.
- Grubb BP: The Postural Tachycardia Syndrome: When to Consider it in Adolescents. Family Practice Recertification 2006;28:19-30
- Khalil K, Saeed B, Karabin B, et al. Clinical Presentation and Management of Patients with Hyperadrenergic Postural Orthostatic Tachycardia Syndrome. A Single Center Experience. Cardiol J 2011;18:1-5.
- Shannon JR, Flattem NL, Jordan J, Jacob G et al. Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency N Engl J Med. 2000 Feb 24;342(8):541-9.
- Mathias CJ, Low DA, Iodice V et al. Postural tachycardia syndrome--current experience and concepts. Nat Rev Neurol. 2011 Dec 6;8(1):22-34. doi: 10.1038/nrneurol.2011.187.
- Kanjwal K, Saeed B, Karabin B et al. Comparative clinical profile of postural orthostatic tachycardia patients with and without joint hypermobility syndrome. Indian Pacing Electrophysiol J. 2010 Apr 1;10(4):173-8.
- Grubb BP: Postural Tachycardia Syndrome. Circulation 2008;117:2814-2817
- Kanjwal K, Karabin B, Kanjwal Y et al. Autonomic dysfunction presenting as postural orthostatic tachycardia syndrome in patients with multiple sclerosis.Int J Med Sci. 2010 Mar 11;7:62-7.
- Parsaik A, Allison TG, Singer W et al. Deconditioning in patients with orthostatic intolerance Neurology. 2012 Oct 2;79(14):1435-9.
- Raj SR, Robertson D. Blood volume perturbations in the postural tachycardia syndrome. Am J Med Sci 2007;334:57–60.
- Freitas J, Santos R, Azevedo E, et al.Clinical improvement in patients with orthostatic intolerance after treatment with bisoprolol and fludrocortisone. Clin Auton Res. 2000 Oct;10(5):293-9.
- Hoeldtke RD, Bryner KD, Hoeldtke ME, et al. Treatment of postural tachycardia syndrome: a comparison of octreotide and midodrine.Clin Auton Res. 2006 Dec;16(6):390-5. Epub 2006 Oct 11.
- Chen L, Wang L, Sun J, et al.Midodrine hydrochloride is effective in the treatment of children with postural orthostatic tachycardia syndrome. Circ J. 2011;75(4):927-31. Epub 2011 Feb 2.
- Kanjwal K, Karabin B, Sheikh M, et al. Pyridostigmine in the treatment of postural orthostatic tachycardia: a single-center experience. Pacing Clin Electrophysiol. 2011 Jun;34(6):750-5
- Kanjwal K, Saeed B, Karabin B, et al.Erythropoietin in the treatment of postural orthostatic tachycardia syndrome. Am J Ther. 2012 Mar;19(2):92-5.
- Lai CC, Fischer PR, Brands CK, et al. Outcomes in adolescents with postural orthostatic tachycardia syndrome treated with midodrine and beta-blockers.Pacing Clin Electrophysiol. 2009 Feb;32(2):234-8.
- Alexandra Sousa, Ana Lebreiro, Joa˜o Freitas, et al. Long-term follow-up of patients with postural tachycardia syndrome. Clin Auton Res (2012) 22:151–153

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




