Pictorial essay: central venous catheters on chest radiographs
Krishnan Melarkode and M Y Latoo
Cite this article as: BJMP 2009:2(2) 55-56
|
Chest radiographs are one of the most common radiological procedures performed in medical practice. The chest radiograph should ideally include views of the heart, lungs, trachea, mediastinum, bones of the chest and upper part of the abdomen. Chest radiographs are normally taken in the posterior-anterior (PA) view with the patient in upright / standing position but for patients admitted in the intensive care unit (ICU) or other emergency situations, this is not possible and so they are taken in the supine (anterior-posterior views) or semi-erect position.
Chest radiographs are done not only for diagnostic reasons to look for abnormalities in the lungs, soft tissues and bones but also to check the position of various invasive lines and tubes. In this article, we aim to discuss and compare the normal and abnormal positions of central venous catheter (CVC) on chest radiographs.
Indications for Central Venous Catheter (Internal Jugular Vein Cannulation)
There are many indications for central venous cannulation 1. These include:
- Central venous pressure (CVP) monitoring
- Pulmonary artery catheterisation and monitoring
- Transvenous cardiac pacing
- Administration of drugs (vasoactive drugs, chemotherapy etc)
- Aspiration of air emboli
- Administration of fluids (in case of difficult peripheral venous access)
Confirming the position of the central venous catheter tip:
For accurate CVP measurement, the tip of the central venous catheter (CVC) should lie within the superior vein cava (SVC), above its junction with the right atrium and parallel to the vessel walls 1. After insertion of a CVC, the position of the catheter tip must be confirmed radiologically, as catheter tips located within the heart can cause cardiac perforation and tamponade 1. Hence, optimum positioning of the CVC tip is required to prevent complications.
If the CVC tip is situated high up (above the pericardial reflection), this can cause vessel wall erosion and if they are very low (in the right atrium), they can cause arrhythmias, placement in the coronary sinus and damage to the tricuspid valve 2.
The carina is a useful radiological landmark for CVC tip position. In this edition of pictorial essay, we aim to discuss the optimum position of both the right and left sided IJV cannula on chest radiographs.
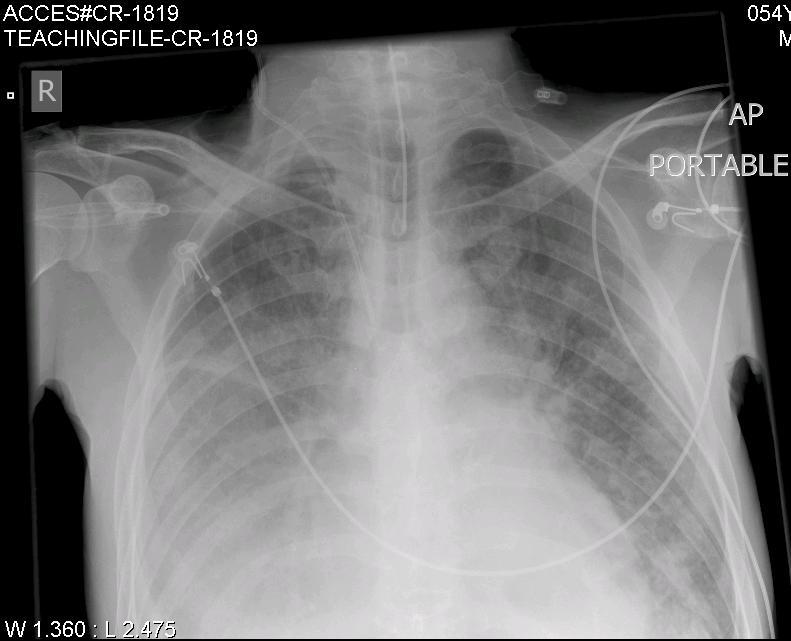
Fig: 1 (CR-1819) shows the normal position of a right sided IJV catheter. The tip of the right sided IJV cannula should ideally lie just above the level of the carina 2. This is the junction of the left and right innominate veins with the superior vena cava (SVC).
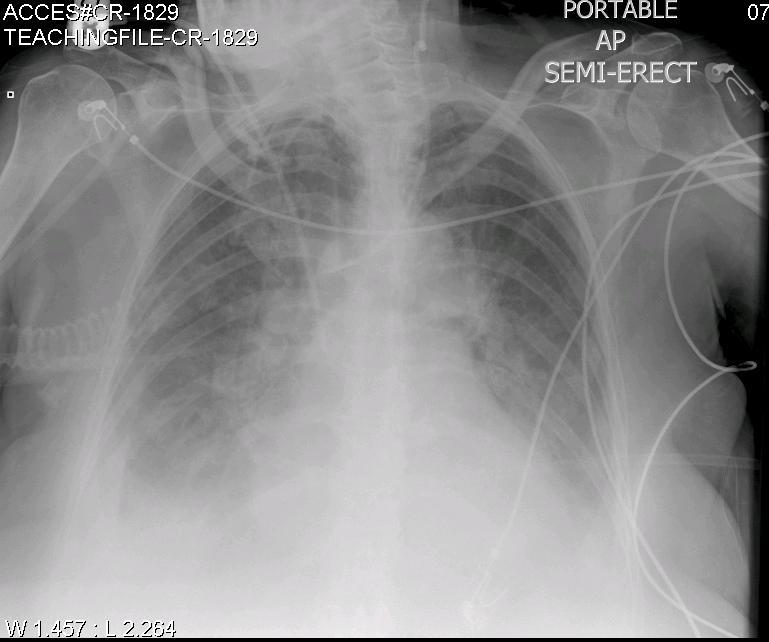
Fig: 2 (CR-1829): The optimum position of the left sided IJV cannula is at or just below the level of the carina 2. This radiograph shows the comparison between the right and left sided IJV cannula in the same patient.
The right sided IJV cannula is too low (below the level of the carina) and is probably in the right atrium while the tip of the left sided IJV cannula is optimally placed.
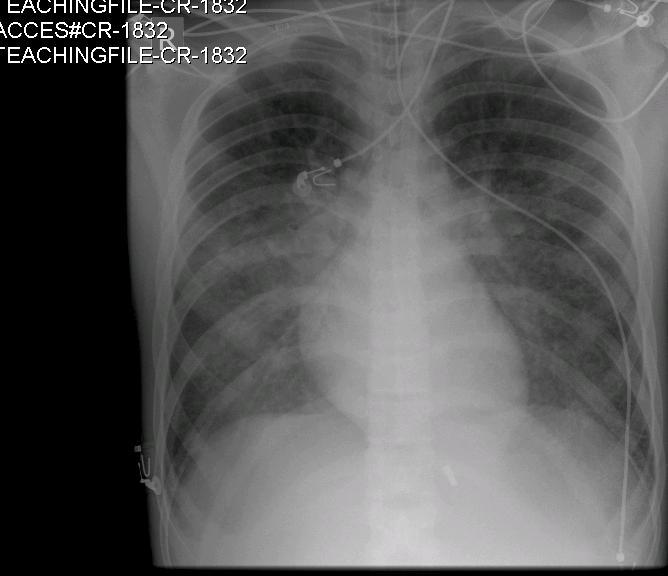
Fig: 3 (CR-1832): In this radiograph, the right sided IJV cannula is too high in the neck. This will not give an accurate CVP measurement. Besides, there is also a risk that the CVC might get dislodged and lead to extravasation of administered fluids and drugs.
Seldinger technique for CVC insertions:
The CVC’s are usually inserted using the Seldinger technique. The IJV can be located by using anatomical landmarks or under direct vision with the help of an ultrasound machine. In the Seldinger technique, after puncture of the IJV, a thin J-shaped guide wire is introduced through the puncture needle. The needle is then slowly withdrawn leaving the J-shaped guide wire in place. A dilator is then introduced over the guide wire to dilate the skin and the subcutaneous tissue. Next, the dilator is removed and the CVC is introduced over the guide wire. Finally, it is important that the guide wire is removed and the CVC is secured.
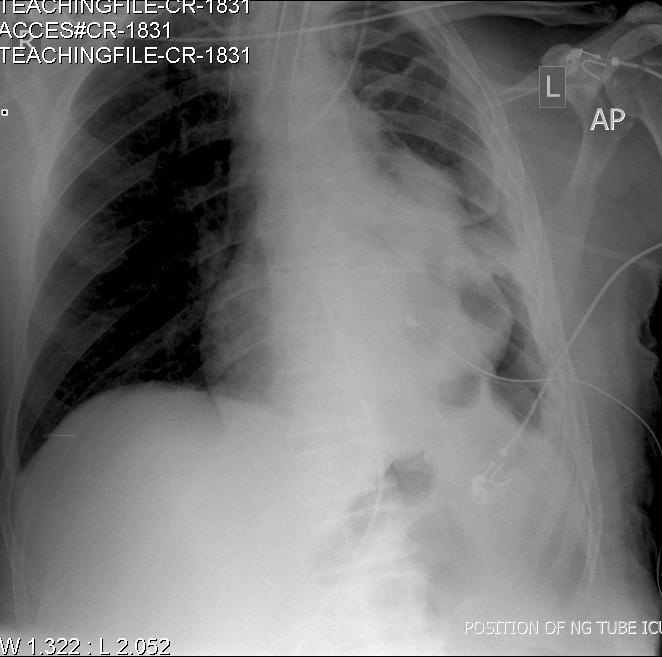
Fig: 4 (CR-1831). This chest radiograph shows an unusual complication where the guide wire has been left accidentally in situ on the right side. (Note the presence of the J-shaped guide wire on the right side of the neck). This can result in serious complications if the guide wire migrates distally.
Conclusion:
In this article, we have highlighted the optimum placement of central venous catheters on chest radiographs. It is imperative that after every CVC insertion (via the IJV or subclavian vein), the position of the tip be confirmed radiologically and if any re-positioning is required, it must be done. The above discussion is true for even CVC’s inserted through the subclavian veins.
Self Assessment
MCQ:
The tip of the right sided IJV cannula should be located
a. below the level of the carina
b. at the level of the clavicle
c. just above the level of the carina
d. in the right atrium
Answer: c
| ACKNOWLEDGEMENTS We wish to thank the Department of Radiology in Bedford Hospital for helping us with the chest radiographs. COMPETING INTERESTS None Declared AUTHOR DETAILS DR. KRISHNAN MELARKODE, MD DNB FRCA, Specialist Registrar in Anaesthesia, Bedford Hospital NHS Trust, UK DR. M Y LATOO, MBBS FRCA, Consultant Anaesthetist, Bedford Hospital NHS Trust, UK CORRESPONDENCE: Dr. Krishnan Melarkode, Specialist Registrar in Anaesthesia, Bedford Hospital, Bedford, UK Email: drkrishnanmr@gmail.com |
References
- Mark JB, Slaughter TF and Gerald Reves J. Cardiovascular monitoring. In: Miller RD ed. Anesthesia. 5th edition. Churchill Livingstone; 1144-51.
- Stonelake PA and Bodenham AR. The carina as a radiological landmark for central venous catheter tip position. British Journal of Anaesthesia 2006; 96: 335-340

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

